

Essay on Diseases
Students are often asked to write an essay on Diseases in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Diseases
Understanding diseases.
Diseases are health conditions that cause discomfort or pain. They can be caused by various factors like germs, unhealthy lifestyle, or genetics.
Types of Diseases
Diseases are of two types: infectious and non-infectious. Infectious diseases spread from person to person, while non-infectious don’t.
Prevention of Diseases
Prevention is better than cure. Healthy habits like eating balanced meals, exercising regularly, and maintaining hygiene can prevent diseases.
Treatment of Diseases
Treatment depends on the type of disease. Some need medicines, others need lifestyle changes, and some may need surgery. Always consult a doctor for treatment.
250 Words Essay on Diseases
Introduction.
Diseases, a ubiquitous part of life, are disruptions to the normal functioning of organisms, particularly humans. They are a complex phenomenon, interweaving biological, environmental, and social factors.
Diseases can be broadly categorized into infectious and non-infectious. Infectious diseases are caused by pathogens such as bacteria, viruses, and parasites. They are transmissible, often leading to epidemics or pandemics, such as COVID-19. On the other hand, non-infectious diseases, including heart disease and diabetes, are typically caused by genetic predispositions, lifestyle choices, or environmental factors.
Impact of Diseases
The impact of diseases extends beyond the individual, affecting families, communities, and entire nations. They can cripple economies, strain healthcare systems, and disrupt social structures. Moreover, diseases often exacerbate existing inequalities, disproportionately affecting vulnerable populations.
Prevention and Treatment
Prevention and treatment of diseases involve a multi-pronged approach. This includes public health measures, medical interventions, and individual behaviors. Vaccination, sanitation, and education are crucial in preventing infectious diseases. Lifestyle modifications and medications play a significant role in managing non-infectious diseases.
In conclusion, diseases are a significant challenge to global health, necessitating concerted efforts for prevention, treatment, and management. The study of diseases, therefore, is not just a biological or medical endeavor, but also a social and political one.
500 Words Essay on Diseases
Diseases, broadly defined, are conditions that impair normal tissue function. They can be caused by a variety of factors, including genetic anomalies, environmental toxins, and infectious agents, among others. Understanding the nature and mechanics of diseases is crucial in developing effective prevention, diagnosis, and treatment strategies.
Classification of Diseases
Diseases are classified into two main categories: infectious and non-infectious. Infectious diseases are caused by pathogens such as bacteria, viruses, fungi, and parasites. They are often transmissible from one organism to another, either directly or indirectly. Examples include influenza, tuberculosis, and malaria.
Non-infectious diseases, on the other hand, are not caused by infectious agents and are not transmissible. They can be caused by a variety of factors, including genetic predisposition, lifestyle choices, and environmental factors. Examples include heart disease, diabetes, and cancer.
Pathogenesis of Diseases
The pathogenesis of a disease refers to the biological mechanism that leads to the diseased state. It involves studying the interaction between the host’s cellular functions and the damaging agent. Understanding the pathogenesis of a disease is crucial for identifying potential targets for therapeutic intervention.
For instance, the pathogenesis of cancer involves the accumulation of genetic mutations that lead to uncontrolled cell growth. By understanding these mechanisms, scientists have been able to develop targeted therapies that specifically inhibit these abnormal cellular processes.
Prevention and Control of Diseases
Preventing and controlling diseases is a critical aspect of public health. This can be achieved through a variety of strategies, including vaccination, sanitation, and lifestyle modifications.
Vaccination is a highly effective method of preventing infectious diseases. It involves the administration of a vaccine, which stimulates the body’s immune system to recognize and fight off specific pathogens.
Sanitation measures, such as clean water and proper waste disposal, can also help prevent the spread of infectious diseases. Meanwhile, lifestyle modifications, such as a balanced diet and regular exercise, can help prevent non-infectious diseases.
In conclusion, diseases are a significant challenge to human health and well-being. Their diverse nature, ranging from infectious to non-infectious, and their complex pathogenesis require a multifaceted approach to prevention, diagnosis, and treatment. As we continue to deepen our understanding of diseases, we can develop more effective strategies to combat them and improve overall public health. It is a testament to the importance of continued research and public health efforts in the fight against disease.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on My Favourite Sportsman MS Dhoni
- Essay on Mahendra Singh Dhoni
- Essay on Teenage Depression
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Volume 21 Supplement 6
Spotlight on ICD-11: New Features and New Opportunities
- Open access
- Published: 09 November 2021
ICD-11: an international classification of diseases for the twenty-first century
- James E. Harrison ORCID: orcid.org/0000-0001-9893-8491 1 ,
- Stefanie Weber 2 ,
- Robert Jakob 3 &
- Christopher G. Chute 4
BMC Medical Informatics and Decision Making volume 21 , Article number: 206 ( 2021 ) Cite this article
116k Accesses
170 Citations
53 Altmetric
Metrics details
The International Classification of Diseases (ICD) has long been the main basis for comparability of statistics on causes of mortality and morbidity between places and over time. This paper provides an overview of the recently completed 11th revision of the ICD, focusing on the main innovations and their implications.
Changes in content reflect knowledge and perspectives on diseases and their causes that have emerged since ICD-10 was developed about 30 years ago. Changes in design and structure reflect the arrival of the networked digital era, for which ICD-11 has been prepared. ICD-11’s information framework comprises a semantic knowledge base (the Foundation), a biomedical ontology linked to the Foundation and classifications derived from the Foundation. ICD-11 for Mortality and Morbidity Statistics (ICD-11-MMS) is the primary derived classification and the main successor to ICD-10. Innovations enabled by the new architecture include an online coding tool (replacing the index and providing additional functions), an application program interface to enable remote access to ICD-11 content and services, enhanced capability to capture and combine clinically relevant characteristics of cases and integrated support for multiple languages.
Conclusions
ICD-11 was adopted by the World Health Assembly in May 2019. Transition to implementation is in progress. ICD-11 can be accessed at icd.who.int.
Understanding diseases in ways that enable prevention, treatment, and the allocation of resources requires measurement. To be useful, measurement must be reliable, allow valid comparisons to be made between places and over time, and enable coherent summarization of large volumes of data. A classification of diseases and related things is essential for such measurement.
For more than a century, the International Classification of Diseases (ICD) has been the main basis for comparable statistics on causes of death and non-fatal disease [ 1 , 2 ]. The 10th revision (ICD-10) was released nearly 30 years ago [ 3 ]. It serves a variety of functions in much of the world—at least 120 countries—and has been translated into 43 languages [ 4 ].
Uses of the ICD are diverse and widespread, extending directly to much of the world and indirectly to all populated places. Much of what is known about the extent, causes and consequences of human disease world-wide rests on use of data classified according to the ICD. Clinical modifications of ICD are the main basis for statistics on disease, particularly cases treated by hospitals. These statistics underlie crucial functions such as payment systems, service planning, administration of quality and safety and health services research.
This essential infrastructure for health information has now been revised for the 11th time. The 11th revision was more extensive and has greater implications for what can be done with the ICD, and how, than any revision since the 6th, in 1948.
Since the development of ICD-10, medicine has advanced, and the understanding of many diseases has changed substantially. The modifications needed to accommodate these changes exceeded what could be achieved by simply updating the 10th revision. Another reason for undertaking a major revision of the ICD is an extrinsic factor, which now affects almost all areas of life: the arrival of the digital age [ 5 ]. While ICD-10 has long been used in digital forms, properties that reflect its pre-digital origin constrain tooling and data exchange, impede maintenance and development, and have enabled differences of structure and meaning to creep into translations and modifications.
The 11th revision [ 6 ], adopted by the 72nd World Health Assembly in May 2019 after extensive consultation and deliberation [ 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 ], addresses these shortcomings of ICD-10 and more. In aggregate, the changes are substantial: ICD-11 is not just ICD-10 with some new categories. Rather, ICD-11 is a different and more powerful health information system, based on formal ontology, designed to be implemented in modern information technology infrastructures, and flexible enough for future modification and use with other classifications and terminologies. It is better able to capture clinically relevant characteristics of cases and to permit summarization of information for various purposes, has flexibility allowing use in more and less elaborate modes, and has integrated support for multiple languages. It is also designed to ensure that data coded according to ICD-11 will be comparable with data coded to ICD-10.
This commentary introduces the conceptual basis for the design of ICD-11 and provides an overview of the content and the most important features.
The design of ICD-11
Information framework.
Fundamental to making the ICD fit for the digital age has been to base it on a computable knowledge framework. This is the most important difference between ICD-11 and earlier revisions. Introduction of a knowledge framework has enabled ICD-11 to be interoperable in digital health information environments. Though ICD-11 can be used in paper-based systems, the tools and capabilities made possible by the framework are expected to make electronic use compelling for most users. The first derived classification, ICD-11 for Mortality and Morbidity Statistics (ICD-11-MMS), is the most direct successor to ICD-10.
The information framework for ICD-11 has three integrated parts: a database referred to as the Foundation, classifications derived from the Foundation, and a common biomedical ontology linked to the Foundation. These components are described below.
The Foundation
The Foundation has about 80,000 entries complemented by 40,000 synonyms, each characterizing a disease, syndrome, or health-related phenomenon in a way that not only is descriptive but also specifies its relationships with other entities and provides a way for digital systems to take account of meaning that may be assigned to an entity. In other words, the Foundation is a semantic network.
A template, or content model [ 22 ], specifies what must be or can be recorded in each entry. Attributes that are well populated on release include a unique, unchanging identifier, preferred name, fully specified name, synonyms, human language translations of names and synonyms, a description (approximating a definition), notes, details of severity grades or stages, parent relationships, and child relationships. The template also includes elements that are more aspirational, such as genomic associations, etiology, clinical criteria and manifestations.
Statistical classifications, such as the ICD-11-MMS, have the property of mutual exclusivity: each codable concept must be located in only one place in the classification’s hierarchy. Many concepts in the ICD have properties that relate them to more than one part of the hierarchy. For example, stroke involves the circulatory system and results in neurological disease. Provision of suitable categories for stroke is more important than where they are placed, though placement is a matter on which strong views sometimes exist [ 23 , 24 ]. The Foundation reduces the impact of such choices by allowing a concept to have many parents.
This property of the Foundation is useful in classifications based on it. For example, while stroke is located in the neurology chapter of ICD-11-MMS, the disease also appears in the cardiovascular chapter (where it was located in ICD-10), with an indication that its primary location is elsewhere. Hence, multiple parenting in the Foundation allows categories to appear in ICD-11 classifications where various users might expect to find them.
Practical considerations dictate that a statistical classification will comprise a limited number of categories, constraining the scope and specificity of the phenomena that can be coded in ICD-11-MMS. The Foundation is practically unlimited in this respect. Specificity implicit in the Foundation that goes beyond that in ICD-11-MMS can be used by other classifications, which are expected to be derived from the Foundation.
Primary authoring of ICD-11 was done in English. However, each preferred term, fully specified term, and synonym is being rendered into the other standard languages of the World Health Organization (WHO)—Arabic, French, Mandarin, Russian, and Spanish—by means of a large multilingual phrase thesaurus, accumulated from translations of previous revisions of the ICD, with trained translators checking the results. Some other languages are also included, and the number will increase as ICD-11 comes into use.
Linearization
As a statistical classification, the ICD-11-MMS has special properties, notably mutual exclusivity of categories, exhaustive coverage of the domain of interest, and arrangement as a single hierarchical tree. In contrast, the Foundation embodies a rich network of relationships between entities, in which there is no constraint on entities having more than one logical parent. That is, many hierarchies are implicit in the Foundation. Deriving this particular statistical classification from the Foundation required use of a process known in information science as linearization [ 25 ].
Linearizing the ICD-11-MMS from the Foundation involved deciding which entities in the Foundation would be included in the classification, deciding on the depth of its hierarchy, and putting each selected entity into a single place in the classification hierarchy. Other classifications can also be linearized from the Foundation (Fig. 1 ). Decisions on which entities to include in each and how to organize the hierarchy can be expected to differ according to the purpose in mind (e.g., a clinical specialty such as dermatology, primary care, or public health). The family of classifications linearized from the Foundation has the special property that mapping or cross-walking between terms can be done reliably.
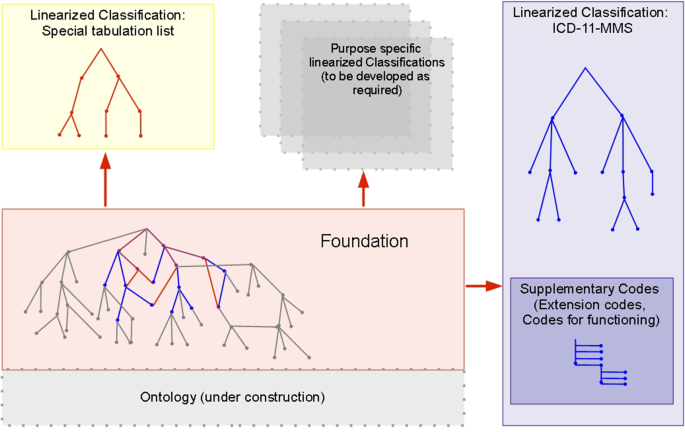
The ICD-11 Foundation and classifications based on it, including ICD-11 for mortality and morbidity statistics (ICD-11-MMS). Many classifications can be linearized from the rich Foundation. ICD-11-MMS (the main classification; blue) and the special tabulation list (a short set of categories for standard summary reports; red) share some concepts in the Foundation (purple). Concepts in the Foundation that are not included in ICD-11-MMS classification (grey) are, nevertheless, part of its index. Practicalities for use of ICD-11-MMS required that it should be constrained to a modest number of codable categories. Great extension of the expressive capabilities of ICD-11-MMS is provided by permitting code clusters to be built by combining stem codes and adding supplementary codes, chiefly extension codes (see Table 1 )
As is typical of statistical classifications, achieving the property of exhaustiveness for ICD-11-MMS required the addition of residual categories (“other specified,” “unspecified”). Residuals are not part of the Foundation and are only meaningful in the context of a particular classification.
Common ontology
The Foundation is a semantic knowledge base. The entities used in the knowledge base, and how they are represented, are referred to by the information science term 'ontology' [ 25 ]. The Foundation can be anchored to external ontology sources by inclusion and reconciliation of terms and definitions, with attribution. Some preliminary demonstrations [ 26 , 27 ] were done with SNOMED [ 28 ], with others planned for the Human Phenotype Ontology [ 29 ] and MedDRA [ 30 ]. Future options may include other members of the Open Biomedical Terminologies (OBO) [ 31 ] community.
The more adequately the ontology underlying ICD-11 represents the relevant domain of knowledge the more straightforward it should be to incorporate new entities. For example, the SARS-CoV-2 virus, the COVID-19 disease, and various manifestations of the disease, which emerged after the release of ICD-11, were easily incorporated as new instances of relevant dimensions of the ICD-11 content model.
In ICD-10 a diagnosis is usually represented by a single code. A limited exception was provided by the dagger-asterisk convention, which allowed a code representing the etiology of a disease (e.g., diabetes) to be linked with a code representing a manifestation (e.g., retinopathy). Likewise, the external causes of injuries are commonly coded as well as their diagnoses. ICD-10 lacks a well-developed infrastructure to support linking of codes, and information for this is often not captured or is lost in processing.
ICD-11-MMS provides a general mechanism to allow codes to be combined to form clusters for use where expressive power is required beyond that provided by any single category (Fig. 2 ). In principle, any ICD-11-MMS category that can be coded on its own (a “stem code”) can also be clustered with one or more other stem codes. A stem code can also be qualified by being clustered with one or more “extension codes”, which can only be used in clusters (Table 1 ). ICD-11-MMS provides over 20,000 extension codes, many of which are of a few types, such as a hierarchical list of drugs and other substances that might cause poisoning, or harm health in other ways. These extension codes allow further specificity and additional information to be added to stem codes.
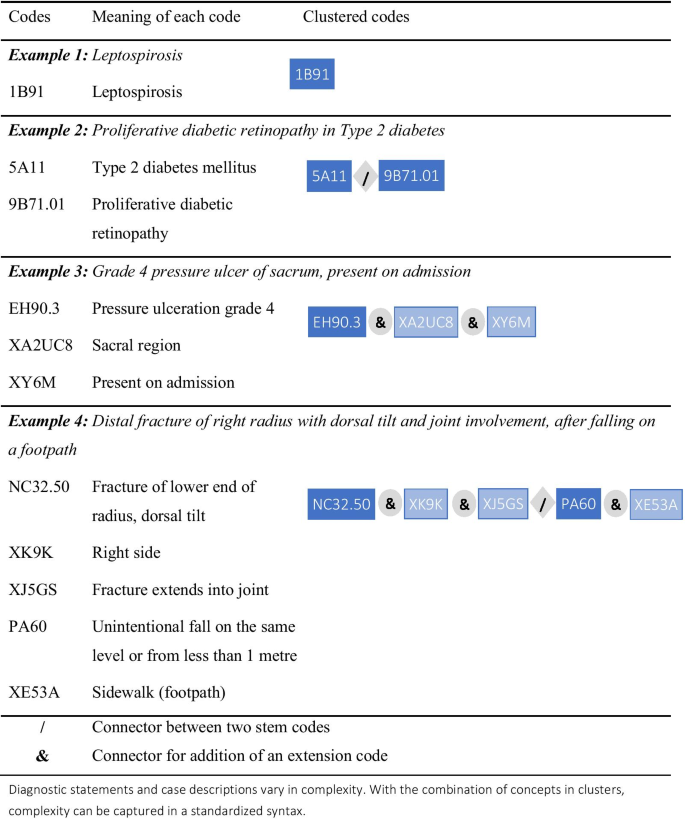
Examples of ICD-11-MMS code clusters
Users and their purposes will determine how much detail is necessary, and ICD-11-MMS provides great flexibility in this regard. While extensive clustering will be necessary to meet the needs of some users, others might require little or none, and ICD-11-MMS has been designed to provide coherent information and the basis for useful statistical comparisons if only a single stem code is assigned to a main diagnosis or underlying cause of death.
Quality and safety of health care exemplifies the potential of clustering. Consider a person admitted to hospital for a surgical procedure who experiences a complication of care. ICD-11-MMS allows for coding of the disease for which surgery was undertaken (that would be the subject of one cluster) and of the complication. A code cluster on the latter can record the harm sustained (e.g., marked nausea and vomiting after surgery), the medication involved (perhaps a particular anesthetic agent), and how the problem came about (e.g., dose too high or too low, or administered at the wrong time). Extension codes can also record whether a condition had been recognized as present when the episode of care began.
Support for digital communication
Every distinct concept in the ICD-11 has been assigned a unique and unchanging identifier. This unique resource identifier (URI) remains the same whether the concept appears solely in the Foundation or is also included in the ICD-11-MMS (or another classification) linearized from the Foundation. The URIs are for use by digital systems and are intentionally “meaningless identifiers” [ 32 ], which enable many of the capabilities of ICD-11. For example, they will enable a health information system to reliably locate information on a topic in any of the languages available on the WHO platform, facilitating health care across borders. The URIs are distinct from ICD-11-MMS codes, which are not arbitrary, reflect aspects of the classification tree, and are for use by humans.
ICD-11 is a unique knowledge base of diagnostic concepts and related matters. The URIs identify the numerous entities within it but do not, on their own, provide users with a way to tap its potential. To enable that, the WHO has created a suite of application programming interfaces (APIs), or RESTful web resources [ 33 ]. These will allow developers anywhere to integrate access to ICD-11 and its services into software, such as coding support applications, and to use the URI to retain the exact detail of a term in addition to the statistical code or code combinations.
Coding tool as index
Use of the index volume is the recommended way to find the appropriate code for a disease in ICD-10 and earlier revisions [ 34 ]. ICD-11 provides users with a different way to find and select categories. The digital capabilities described above have been used by the WHO to create a web-based coding tool [ 35 ] that employs partial word-matching, word-order independence, synonym management, hierarchy traversal, and more. Where a search term equates to a cluster, rather than to a single stem code, the tool can return the assembled cluster.
Application prototypes using the ICD-11 API have been demonstrated for mobile devices, making electronic access to ICD coding available just about anywhere. Low-resource areas and sites will be able to use these free resources with inexpensive devices, which are likely to be less costly and more portable than bulky printed volumes and indices. Field testing of the coding tool and system show promising indications that it will result in more comparable, consistent, and accurate coding than did the previous approach.
Current medical knowledge
The need to accommodate new knowledge about diseases and changes in related concepts and terms necessitated many changes in the ICD. In fact, the need for updates was noted soon after ICD-10 was published. An updating mechanism was put into place, but structural characteristics of ICD-10 and requirements for continuity limited the types of changes that could be made, and a growing list of desired changes were put aside for the 11th revision.
A design objective for the 11th revision was to maintain good backwards comparability with ICD-10, particularly for important conditions, and changes were made only where credible reasons emerged to do so. Despite the many changes at specific levels, the overall framing of diseases in ICD-11-MMS remains similar to that in ICD-10, and this is reflected in the similar titles and sequence of chapters. Several new chapters and sections have been added for various reasons (Table 2 ). Specific changes include the addition of categories for new concepts, splitting and lumping of old categories, retirement of redundant categories, rewording of titles, and movement of categories from one place to another within the classification tree.
Acute myocardial infarction provides an example of how the 11th revision has affected coverage of an important cause of mortality and morbidity (Fig. 3 ). ICD-11-MMS provides a stem code with the same name and scope as that in ICD-10, to ensure that statistical time trends are comparable from ICD-10 to ICD-11-MMS. The WHO accepted advice that it is better to provide subcategories that are specified in terms of the presence of acute ST elevation than in terms of the affected part of the myocardium. It remains possible to code the part affected, but that is now done by adding an extension code to the code cluster representing the condition.
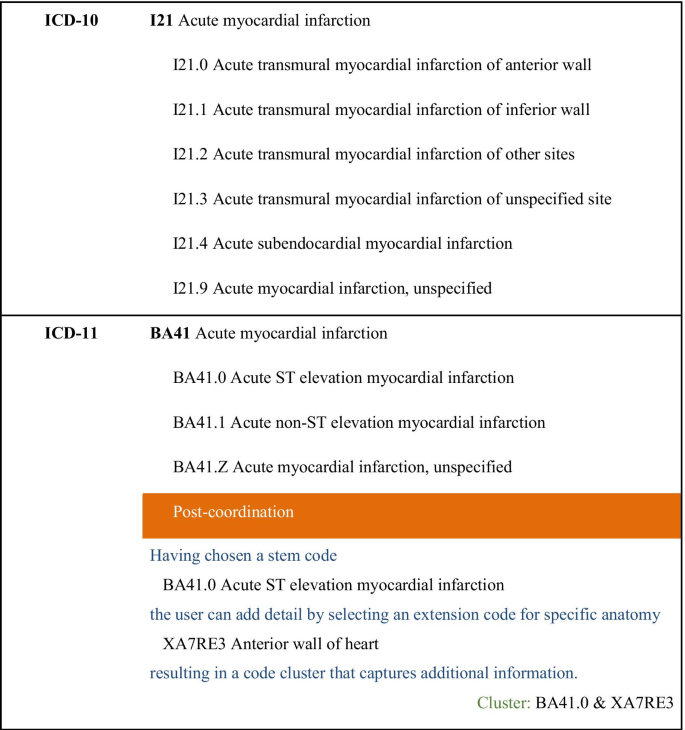
Acute myocardial infarction in ICD-10 and ICD-11-MMS
Expected benefits of ICD-11-MMS
The new revision was designed to be capable of replacing all functions of ICD-10. In many contexts it will be capable of providing additional services or will provide existing functions in an improved way. This section describes what is expected in several areas.
Global reach, accessibility, and standardization
ICD-10 is used in many countries but little, if at all, in some others. The digital and web-based design of ICD-11-MMS will reduce certain barriers to wider use of the ICD [ 36 ]. The enhanced language support, the coding tool, the API on which it is based, and the applications that are expected to tap the potential of the API will make it easy for a person anywhere with web access to have essentially equivalent access to exactly the same version of ICD-11-MMS. Networks of ICD user agencies and individuals that exist in the era of ICD-10 are expected to develop further on the back of the inherently networked ICD-11-MMS.
Health metrics
For many decades, ICD-coded data have been the basis for international and national statistics on cause-specific mortality [ 37 ]. More recently, the mortality data, along with ICD-coded morbidity data, have been crucial inputs to estimates of burden of disease and injury at a global level [ 38 ] and more locally [ 39 ].
These measures commonly deal with fairly broad types of causes (e.g., tuberculosis, suicide), and ICD-11-MMS has been designed to provide statistical continuity for major causes as well as many specific causes. For example, the 264 causes [ 40 ] investigated in the Global Burden of Disease Study on the basis of data coded to ICD-10 and earlier revisions can be replicated using data coded to ICD-11-MMS. Mapping tables provided by the WHO will help to compile the same disease groups.
Some topics will be affected by the revision, particularly where category scope or placement have changed, or the basis for specifying subgroups. For example, statistics on the occurrence of transmural and subendothelial myocardial infarctions over time will be affected by the changes described in Fig. 3 unless all ICD-11-MMS data incorporate the anatomy extension code. Detailed analysis and bridge-coding studies [ 41 ] could assist in evaluating the impact of changes and provide a basis to allow for effects of the revision when interpreting statistics.
Integrated support for hospital case data
The ICD has long been used to code records of hospital-admitted patients and some other types of clinical records. Many users found that the version of ICD-10 published by the WHO provided insufficient specificity for clinical purposes and for the related purpose of supporting activity-based billing and funding systems. Some WHO member countries developed “clinical modifications” of the ICD to serve these purposes. While similar in some respects, the various clinical modifications also differ considerably and do not provide an adequate basis for international comparisons [ 42 ].
ICD-11-MMS has been designed with these clinical purposes in mind, as well as mortality coding. Some parts of ICD-11-MMS draw on the clinical modifications of ICD-10 (e.g., the injury chapter), and the ICD-11 Foundation includes all categories that exist in the main clinical modifications of ICD-10. While WHO member states have yet to fully assess the sufficiency of ICD-11-MMS for these purposes, it is hoped that it will meet their requirements with much less need for modification than ICD-10 has, if any. Hence, ICD-11-MMS will facilitate international standardization of morbidity data in a way that ICD-10 could not.
Capability to operate within health information systems
The digital underpinning of ICD-11-MMS makes it a “native citizen” of the era of networked interoperating health information systems. Increasingly, data with different origins are combined for administrative or research purposes, enabling more value to be obtained from existing data. Where the sources combined include, for example, mortality and morbidity data, analysis and interpretation will be facilitated when the data in both sources are classified according to ICD-11-MMS.
As a classification designed with input from clinicians and agencies responsible for providing and administering health care, ICD-11-MMS is uniquely adapted to enable coherent and useful summarization of large volumes of disease data [ 43 ]. The data may originate in manual or electronic health records and be coded directly to ICD-11-MMS or via a structured terminology, such as SNOMED CT.
ICD-11-MMS support for activity-based funding systems
Activity-based systems, widely used to administer and allocate funds for hospital care, rely on coded diagnosis data [ 44 , 45 ]. The similarities between ICD-10 and ICD-11-MMS and the great expressive potential of the new revision are reasons to expect that ICD-11-MMS will provide a good basis for activity-based systems. Rules on the extent of detail to be coded in a system may be needed to ensure that application of ICD-11-MMS results in minimal, if any, increase in coding burden, while tapping its flexibility and granularity. Once activity-based systems have migrated to ICD-11-MMS, greater international comparability may be achieved.
Quantitative derived measures
Case mix cost weights are long-established quantitative measures derived largely from ICD-coded data [ 46 ]. Other ICD-based quantitative derived measures have emerged, including measures of the probability of survival to discharge [ 47 ] and the presence of persisting disability after injury [ 48 ]. The great expressive power of ICD-11-MMS, particularly concerning aspects of case severity, is expected to support better performing quantitative measures on a wider range of topics.
Governance, maintenance, and updates
We anticipate that preparations for implementation of ICD-11-MMS in a variety of settings will reveal some omissions and other potential for improvement that were not detected during pre-release testing. Naturally, new knowledge about diseases will also necessitate changes for as long as ICD-11-MMS is in use. The WHO has established two groups that will work together and with the WHO to maintain and update ICD-11: a Medical and Scientific Advisory Committee, comprised of medical and scientific experts, who validate the clinical and physiological basis as well as the ontological positioning of proposed entries into the Foundation, and a Classification and Statistics Advisory Committee, which will check proposals for their fitness for integration into the ICD-11-MMS classification and consider their possible impact on coding and coded data. The process for updating ICD-11 will be transparent and open. Anyone can lodge a proposal for updates through an online platform. The flexibility of the structure of ICD-11, combined with this updating mechanism, might obviate the need for another major revision for a considerable time.
Next steps for countries
The adoption of ICD-11 in May 2019 marked the start of an implementation phase by WHO member states. In 2022, reporting of mortality data according to ICD-11-MMS will commence, with a transition period of at least five years. The nature, timing, and complexity of implementation for morbidity coding will vary from place to place. In general, the transition will be most complex in places in which ICD is used widely, in multiple systems, and underlies processes such as activity-based funding. The countries that are first to adopt ICD-11-MMS may well be some that do not have substantial legacy systems that will require alteration to accommodate the revision.
Changes in content reflect developments in the understanding of diseases since ICD-10 was written. The ICD-11 rules for combining categories enable much better description of cases than has been possible previously, and its governance arrangements will ensure that it remains current. Information systems have changed more since ICD-10 was released than in the previous century. The era of globally networked and nearly real-time data systems has transformed many aspects of life, but health information has yet to fully make the transition. From its Foundation, information framework, and API to the suite of user-facing tools, ICD-11 has been designed to enable that transition to occur now. ICD-11 can be accessed at icd.who.int.
Availability of data and materials
ICD-11 can be accessed at icd.who.int.
Abbreviations
Application programming interface
- International classification of diseases
International classification of diseases, 10th revision
International classification of diseases, 11th revision
ICD-11 for mortality and morbidity statistics
Unique resource identifier
World Health Organization
Wood PH. Applications of the international classification of diseases. World Health Stat Q. 1990;43:263–8.
CAS PubMed Google Scholar
World Health Organization. World health statistics. 2020. http://www.who.int/gho/publications/world_health_statistics/en . Accessed 12 Nov 2020
World Health Organization. History of the development of the ICD. http://www.who.int/classifications/icd/en/HistoryOfICD.pdf . Accessed 12 Nov 2020.
World Health Organization. International Classification of Diseases (ICD). https://www.who.int/standards/classifications/classification-of-diseases . Accessed 27 May 2021.
White A. Digital media and society: transforming economics, politics and social practices. New York: Palgrave Macmillan; 2014.
Book Google Scholar
World Health Organization. ICD-11 revision. https://icd.who.int/en . Accessed 12 Nov 2020.
World Health Organization. ICD-11 Revision Conference. Tokyo Japan; 12–14 Oct 2016.
Ghali WA, Pincus HA, Southern DA, Brien SE, Romano PS, Burnand B, et al. ICD-11 for quality and safety: overview of the WHO quality and safety Topic Advisory Group. Int J Qual Health Care. 2013;25:621–5.
World Health Organization. Groups that were involved in ICD-11 Revision Process. https://www.who.int/standards/classifications/classification-of-diseases/groups-that-were-involved-in-icd-11-revision-process . Accessed 28 May 2021.
World Health Organization. ICD-11-MMS Joint Task Force (JTF). 2018. http://www.who.int/classifications/icd/revision/JTF_LOP.pdf . Accessed 12 Nov 2020.
Reed GM, Roberts MC, Keeley J, Hooppell C, Matsumoto C, Sharan P. Mental health professionals’ natural taxonomies of mental disorders: implications for the clinical utility of the ICD-11 and the DSM 5. J Clin Psychol. 2013;69:1191–212.
Article Google Scholar
Roberts MC, Reed GM, Medina-Mora ME, Keeley JW, Sharan P, Johnson DK. A global clinicians’ map of mental disorders to improve ICD-11: analysing meta-structure to enhance clinical utility. Int Rev Psychiatry. 2012;24:578–90.
Stone J, Hallett M, Carson A, Bergen D, Shakir R. Functional disorders in the neurology section of ICD-11: a landmark opportunity. Neurology. 2014;83:2299–301.
Rajakulendran S, Dua T, Harper M, Shakir R. The classification of neurological disorders in the 11th revision of the International Classification of Diseases (ICD-11). J Neurol Neurosurg Psychiatry. 2014;85:972–3.
Aymé S, Bellet B, Rath A. Rare diseases in ICD11: making rare diseases visible in health information systems through appropriate coding. Orphanet J Rare Dis. 2015;10:35.
Chute CG. The rendering of human phenotype and rare diseases in ICD-11. J Inherit Metab Dis. 2018. https://doi.org/10.1007/s10545-018-0172-5 .
Article PubMed PubMed Central Google Scholar
Southern DA, Pincus HA, Romano PS, Bernard B, Harrison J, Forster AJ, et al. Enhanced capture of healthcare-related harms and injuries in the 11th revision of the International Classification of Diseases (ICD-11). Int J Qual Health Care. 2016;28:136–42.
McKenzie K, Fingerhut L, Walker S, Harrison A, Harrison JE. Classifying external causes of injury: history, current approaches, and future directions. Epidemiol Rev. 2012;34:4–16.
Tanno LK, Calderon M, Linzer JF Sr, Chalmers RJG, Demoly P. Joint Allergy Academies. Collaboration between specialties for respiratory allergies in the International Classification of Diseases (ICD)-11. Respir Res. 2017;18:34.
Tanno LK, Chalmers RJG, Calderon MA, Aymé S, Demoly P. On behalf the Joint Allergy Academies. Reaching multidisciplinary consensus on classification of anaphylaxis for the eleventh revision of the World Health Organization’s (WHO) International Classification of Diseases (ICD-11). Orphanet J Rare Dis. 2017;12:53.
World Health Organization. WHO Family of International Classifications (WHO-FIC) Network. 2018. http://www.who.int/classifications/network/en . Accessed 17 Nov 2020.
World Health Organization. ICD11 Content Model Reference Guide. https://icd.who.int/icdapi/docs/ContentModelGuide.pdf . Accessed 28 May 2021.
Shakir R, Davis S, Norrving B, Grisold W, Carroll WM, Feigin V, Hachinski V. Revising the ICD: stroke is a brain disease. Lancet. 2016;388:2475–6.
Boerma T, Harrison J, Jakob R, Mathers C, Schmider A, Weber S. Revising the ICD: explaining the WHO approach. Lancet. 2016;388:2476–7.
Rector A, Schulz S, Rodrigues JM, Chute CG, Solbrig H. On beyond Gruber: “Ontologies” in today’s biomedical information systems and the limits of OWL. J Biomed Inform X. 2019;2:100002. https://doi.org/10.1016/j.yjbinx.2019.100002 .
Rodrigues J-M, Schulz S, Rector A, Spackman K, Millar J, Campbell J, et al. ICD-11 and SNOMED CT common ontology: circulatory system. Stud Health Technol Inform. 2014;205:1043–7.
PubMed Google Scholar
Schulz S, Rodrigues J-M, Rector A, Spackman K, Campbell J, Ustün B, et al. What’s in a class? Lessons learnt from the ICD—SNOMED CT harmonisation. Stud Health Technol Inform. 2014;205:1038–42.
SNOMED International. http://www.snomed.org/ Accessed 17 Nov 2020
The Human Phenotype Ontology. https://hpo.jax.org/app/ Accessed 17 Nov 2020
Harrison J, Mozzicato P. MedDRA®: the tale of a terminology: side effects of drugs essay. Side Effects Drugs Annual. 2009;31:33–41. https://doi.org/10.1016/S0378-6080(09)03160-2 .
The Open Biological and Biomedical Ontology (OBO) Foundry. http://www.obofoundry.org/ Accessed 17 Nov 2020
Cimino JJ. Desiderata for controlled medical vocabularies in the twenty-first century. Methods Inf Med. 1998;37:394–403.
Article CAS Google Scholar
World Health Organization. ICD APIs. https://icd.who.int/icdapi . Accessed 17 Nov 2020.
World Health Organization. International Statistical Classification of Diseases and Related Health Problems—10th revision: Volume 2—instruction manual (2nd ed.). Geneva: World Health Organization; 2004.
World Health Organization. ICD-11 coding tool. https://icd.who.int/ct11/icd11_mms/en/release . Accessed 12 Nov 2020.
WHO. World Health Statistics 2020: Monitoring Health for the Sustainable Development Goals. Geneva, 2020. https://apps.who.int/iris/bitstream/handle/10665/332070/9789240005105-eng.pdf Accessed 25 Feb 2021.
Lancet T. Life, death, and disability in 2016. Lancet. 2017;390:1083.
Lancet T. The Global Burden of Disease Study 2019. Lancet. 2020;396:1129–306.
Australian Institute of Health and Welfare. Australian Burden of Disease Study: impact and causes of illness and injury in Australia 2015. Australian Burden of Disease Study. Canberra: AIHW; 2019.
GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1151–210.
Brocco S, Vercellino P, Goldoni C, Alba N, Gatti M, et al. «Bridge Coding» ICD-9, ICD-10 and effects on mortality statistics. Epidemiol Prev. 2010;34:109–19.
Jetté N, Quan H, Hemmelgarn B, Drosler S, Maass C, Moskal L, et al. The development, evolution, and modifications of ICD-10: challenges to the international comparability of morbidity data. Med Care. 2010;48:1105–10.
Chen D, Zhang R, Zhao H, Feng J. Bibliometric analysis of the development of ICD-11 in medical informatics. J Healthc Eng. 2019. https://doi.org/10.1155/2019/1649363 .
O’Reilly J, Busse R, Häkkinen U, Or Z, Street A, Wiley M. Paying for hospital care: the experience with implementing activity-based funding in five European countries. Health Econ Policy Law. 2012;7(1):73–101. https://doi.org/10.1017/S1744133111000314 .
Article PubMed Google Scholar
Palmer KS, Agoritsas T, Martin D, Scott T, Mulla SM, Miller AP, et al. Activity-based funding of hospitals and its impact on mortality, readmission, discharge destination, severity of illness, and volume of care: a systematic review and meta-analysis. PLoS ONE. 2014;9(10):e109975. https://doi.org/10.1371/journal.pone.0109975 .
Article CAS PubMed PubMed Central Google Scholar
Pettengill J, Vertrees J. Reliability and validity in hospital case-mix measurement. Health Care Financ Rev. 1982;4(2):101–28.
CAS PubMed PubMed Central Google Scholar
Gagné M, Moore L, Beaudoin C, Batomen Kuimi BL, Sirois M-J. Performance of International Classification of Diseases-based injury severity measures used to predict in-hospital mortality: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2016;80:419–26.
Gabbe BJ, Lyons RA, Simpson PM, Rivara FP, Ameratunga S, Polinder S, et al. Disability weights based on patient-reported data from a multinational injury cohort. Bull World Health Organ. 2016;94:806–16.
Download references
Acknowledgements
Many people in addition to the named authors contributed to the 11th revision of the ICD, variously as members of expert and advisory groups, technical and administrative staff, consultants, contractors, reviewers and editors.
About this supplement
This article has been published as part of BMC Medical Informatics and Decision Making Volume 21 Supplement 6 2021: Spotlight on ICD-11: New Features and New Opportunities. The full contents of the supplement are available at https://bmcmedinformdecismak.biomedcentral.com/articles/supplements/volume-21-supplement-6 .
The work resulting in this paper was not supported by a particular grant. The group at Flinders University led by JEH received funds from the Australian Institute for Health and Welfare, which partly supported his contributions to revising the ICD. SW has been employed by the Institute of Medical Documentation and Information (DIMDI), a German government agency responsible for health classifications, including the ICD. DIMDI was merged with the Federal Institute for Drugs and Medical Devices in May 2020. RJ is employed by the WHO. He has been the team leader of the group responsible for the ICD since 2015 and was a member of the team before that. CGC is faculty at Johns Hopkins and previously worked at Mayo Clinic. His work has been supported by multiple grants from the National Institutes of Health. University discretionary funds have supported his WHO work in part.
Author information
Authors and affiliations.
College of Medicine and Public Health, Flinders University, Adelaide, Australia
James E. Harrison
Federal Institute for Drugs and Medical Devices, Bonn, Germany
Stefanie Weber
World Health Organization, Geneva, Switzerland
Robert Jakob
Schools of Medicine, Public Health and Nursing, JohnsHopkins University, Baltimore, MD, USA
Christopher G. Chute
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the development of ICD-11. JEH, SW and CGC were members or chairpersons of several committees convened by the WHO to advise it on the 11th revision of the ICD. RJ is an employee of the WHO and, in that capacity, he led the revision from 2015 and assisted with it before that. JEH prepared the first draft of this paper. SW, RJ and CGC contributed to the development of the paper by adding to and revising the text over several versions. All authors read and approved the final manuscript.
Corresponding author
Correspondence to James E. Harrison .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
JEH, SW, and CGC are or were members of several committees convened by the WHO to advise it on the 11th revision of the ICD. They received travel support—airline tickets and per diem payments to cover accommodation and other costs—from the WHO to allow attendance at some committee meetings. The total extent of this support for the three authors over about 11 years is estimated to be approximately USD 100,000, mostly for JEH and CGC. The group at Flinders University led by JEH received funds from the Australian Institute for Health and Welfare, which partly supported his contributions to revising the ICD. SW has been employed by the Institute of Medical Documentation and Information (DIMDI), a German government agency responsible for health classifications, including the ICD. She has represented DIMDI in committees and meetings concerning ICD and related matters. DIMDI was merged with the Federal Institute for Drugs and Medical Devices in May 2020. RJ is employed by the WHO. He has been the team leader of the group responsible for the ICD since 2015 and was a member of the team before that. CGC is faculty at Johns Hopkins and previously worked at Mayo Clinic. His work has been supported by multiple grants from the National Institutes of Health. University discretionary funds have supported his WHO work in part.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Joint first author: James E. Harrison and Stefanie Weber
Joint senior author: Robert Jakob and Christopher G. Chute
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Harrison, J.E., Weber, S., Jakob, R. et al. ICD-11: an international classification of diseases for the twenty-first century. BMC Med Inform Decis Mak 21 (Suppl 6), 206 (2021). https://doi.org/10.1186/s12911-021-01534-6
Download citation
Received : 02 December 2020
Accepted : 20 May 2021
Published : 09 November 2021
DOI : https://doi.org/10.1186/s12911-021-01534-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Epidemiology
- Informatics
- Classification
BMC Medical Informatics and Decision Making
ISSN: 1472-6947
- General enquiries: [email protected]
- Types of Diseases
Any disorder or malfunctioning of the body or mind that destroys good health can be called as a disease. The status of health of the body in a disease is said to be compromised. A disease can be caused due to a variety of reasons. Every disease has characteristic symptoms through which we can identify the types of diseases.
Suggested Videos

Classification of Diseases – Types of Diseases
According to a very broad classification, diseases can also be classified under the following – physical diseases, mental diseases, infectious diseases, non- infectious diseases, deficiency diseases, inherited diseases, degenerative diseases, social diseases, self-inflicted diseases.
Depending on certain characteristics, diseases can also be classified as an acute disease where the onset of the disease is sudden, lasts for a short time, with rapid changes; and chronic diseases where the effects of the disease can last for months or years.

Even though the types of diseases can be classified very broadly, the classification of diseases into infectious and non-infectious diseases is considered very apt. Infectious diseases can be easily transmitted from one person to the other while the non-infectious disease cannot be transmitted.
Browse more Topics under Human Health And Diseases
- Health and Diseases
- Immune System
- Antigen and Antibody
- Interferons and Lymphoid Organs
- Disorders of Immune System
- Vaccines and Immunisation
- Drugs and Alcohol Abuse
What Causes Cancer?
Any organism or microorganism that causes a disease is called as a pathogen . A specific disease is caused by a specific pathogen. The infectious diseases are often transmitted by pathogens. These diseases can be spread through contact or proximity, either through air, water, soil or through vectors.
Pathogens can be of different types. They can be either bacteria or virus or fungi or a protozoan or even a helminth. Most of the parasites that are found are pathogens as they cause many diseases in humans.
Some of the bacterial diseases are Syphilis, Pneumonia, Tetanus, and Tuberculosis. Examples of diseases caused by a virus are Chickenpox, Small Pox, Measles, Polio. Fungal infections include Ringworm infection, Athlete’s foot, Yeast infections etc. Malaria is a disease caused by an organism belonging to Protista. Diseases caused by helminths include Ascariasis, Taeniasis etc.

Some Types of Diseases Explained Briefly
It is caused by the bacterium, Salmonella typhi. The pathogen enters the body through contaminated food and water. High fever, weakness, stomach pain, headache, constipation, loss of appetite are the symptoms of this disease. The Widal test confirms this disease.
It is caused by Streptococcus pneumoniae and Haemophilus influenzae bacteria. This disease affects the lungs. The alveoli of the lungs get infected and filled with fluid, causing respiratory problems. This is a disease that is acquired by inhaling the droplets or aerosols that are released by an infected person. The main symptoms include chills, fever, headache, and cough.
Common Cold
The common cold is generally caused by a group of viruses called rhinovirus. The respiratory passage and the nose are commonly infected here. Nasal congestion, discharge, sore throat, cough, hoarseness, tiredness, are some of the associated symptoms of common cold, that can last for up to seven days.
This infection is transmitted when an infected person releases the droplets either through a cough or sneeze. These droplets can be either inhaled directly by other people or can be transmitted with the help of contaminated objects.
How does MRI Scanner Work?
It is a disease caused by a protozoan called Plasmodium. There are different types of malaria caused by different types of species of Plasmodium. Some of the species are Plasmodium vivax, Plasmodium malaria, Plasmodium falciparum. Malignant and fatal malaria is caused by Plasmodium falciparum.
The female Anopheles mosquito is the vector that carries the infectious form of the pathogen into the human body. Therefore, the malarial parasite has two hosts, i.e. human and mosquito to complete its life cycle.
When an infected female Anopheles mosquito bites a human, it transfers the sporozoites of the Plasmodium parasite. These parasites multiply in the liver cells and then attack the RBCs, rupturing them. When RBCs rupture, they release a toxic substance called haemozoin. This toxic substance is responsible for the classic symptoms of malaria – fever associated with chills. The spread of the disease can be controlled by killing the vector, mosquito.

Entamoeba histolytica causes Amoebiasis. It is a protozoan parasite that is present in the large intestine of a human. Amoebiasis is also called as amoebic dysentery. This disease is transmitted by houseflies that carry the parasite from the contaminated faeces of an infected person to any food product, thereby contaminating it. The symptoms include abdominal pain, cramps, constipation, stools with excess mucous etc.
It is a disease that is caused by a helminth, Ascaris lumbricodes, also called the roundworm. It is an intestinal endoparasite found in humans. Muscular pain, internal bleeding, fever, anaemia, intestinal passage blockage are some symptoms of this disease. The infection is spread by contamination of soil, water, plants, etc. as the eggs of the parasite are excreted out through the faecal matter.
Also called as elephantiasis, this disease is characterized by the inflammation of the affected organs. Even genital organs can get affected by this disease. Wuchereria bancrofti and Wucheria malayi are the filarial worms that are responsible for causing this disease. The female Culex mosquito acts as the vector for transmitting the pathogen.
Fungal Diseases
Ringworm infection is caused by Fungi. Some of the Fungi that cause this infection are Microsporum, Trichophyton, and Epidermophyton. It is a very common infectious disease that is characterized by intense itching and dry, scaly lesions on the skin, nails, and scalp. Moisture and heat are the favourable factors that help the fungi grow.
Preventive Measures
The different types of diseases, especially, infectious diseases can be prevented by taking the right measures. Personal and public hygiene play an important role here. Eradication of vectors that carry the pathogens is also an effective preventive measure. Vaccinations also help in tackling many infectious diseases.
Mental Health and the factors that affect it .
Solved Questions For You
Q: Blackwater fever is also known as which of the following?
- Yellow Fever
- Scarlet Fever
- Aestivo-autumnal malaria
- Encephalitis
Ans: The correct option is “C”. Blackwater fever, also called malarial hemoglobinuria or ‘aestevo autumnal malaria’ is a complication of malaria in which the RBCs burst in the bloodstream, (hemolysis) releasing haemoglobin directly into the blood vessels and into the urine, leading to kidney failure.
Customize your course in 30 seconds
Which class are you in.

Human Health and Diseases
- Vaccines and Immunization
- Drugs and Alcohol Abuse
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App


Classification, Disease and Evidence
New Essays in the Philosophy of Medicine
- © 2015
- Philippe Huneman 0 ,
- Gérard Lambert 1 ,
- Marc Silberstein 2
IHPST, CNRS/Université Paris I/ENS, Paris, France
You can also search for this editor in PubMed Google Scholar
Centre Cavaillès, Ecole Normale Supérieure, Paris, France
Éditions matériologiques, paris, france.
- Comprehensive overview of current topics in the Philosophy of Medicine
- Connects current Medicine Practice with Philosophy of Science discussions
- Offers original insights in medical ethics and public heath
- Includes supplementary material: sn.pub/extras
Part of the book series: History, Philosophy and Theory of the Life Sciences (HPTL, volume 7)
15k Accesses
1 Altmetric
This is a preview of subscription content, log in via an institution to check access.
Access this book
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Other ways to access
Licence this eBook for your library
Institutional subscriptions

About this book
This anthology of essays presents a sample of studies from recent philosophy of medicine addressing issues which attempt to answer very general (interdependent) questions: (a) what is a disease and what is health? (b) How do we (causally) explain diseases? (c) And how do we distinguish diseases, i.e. define classes of diseases and recognize that an instance X of disease belongs to a given class B? (d) How do we assess and choose cure/ therapy?
The book is divided into three sections: classification, disease and evidence. In general, attention is focused on statistics in medicine and epidemiology, issues in psychiatry and connecting medicine with evolutionary biology and genetics. Many authors position the theories that they address within their historical contexts.
The nature of health and disease will be addressed in several essays that also touch upon very general questions about the definition of medicine and its status. Several chapters scrutinize classification because of its centrality within philosophical problems raised by medicine and its core position in the philosophical questioning of psychiatry. Specificities of medical explanation have recently come under a new light, particularly because of the rise of statistical methods and several chapters investigate these methods in specific contexts such as epidemiology or meta-analysis of random testing. Taken together this collection addresses the question of how we gather, use and assess evidence for various medical theories.
The rich assortment of disciplines featured also includes epidemiology, parasitology and public health, while technical aspects such as the application of game theory to medical research and the misuse of the DSM in forensic psychiatry are also given an airing. The book addresses more than the construction of medical knowledge, however, adding cogent appraisal of the processes of decision making in medicine and the protocols used to justify therapeutic choices.
Similar content being viewed by others

Disease Entities, Negative Causes, Multifactoriality, and the Naturalness of Disease Classifications. Remarks on Some Philosophical Misperceptions of Medical Pathology

Evidence to Guide Decision Making in Clinical Medicine

Medical Theory and Its Notions of Definition and Explanation
- Concept of disease
- DSM philosophy
- Definition genetic disease
- Diagnostic reasoning
- Disease philosophy
- Dualist epistemology of medicine
- Epistemology of mental illness
- Evidence based medicine
- Function in psychiatric debate
- Genetic disease philosophy
- Misuse of DSM
- Parasitology philosophy
- Philosophy Medicine
- Quality assessment tools for evidence in medicine
- Risk factor in epidemiology
Table of contents (10 chapters)
Front matter, objectivity, scientificity, and the dualist epistemology of medicine.
- Thomas V. Cunningham
The Naturalization of the Concept of Disease
- Maël Lemoine
What Will Psychiatry Become?
- Dominic Murphy
The Function Debate and the Concept of Mental Disorder
- Steeves Demazeux
Emerging Disease and the Evolution of Virulence: The Case of the 1918–1919 Influenza Pandemic
- Pierre-Olivier Méthot, Samuel Alizon
Power, Knowledge, and Laughter: Forensic Psychiatry and the Misuse of the DSM
- Patrick Singy
Defining Genetic Disease
- Catherine Dekeuwer
Causal and Probabilistic Inferences in Diagnostic Reasoning: Historical Insight into the Contemporary Debate
Risk factor and causality in epidemiology.
- Élodie Giroux
Herding QATs: Quality Assessment Tools for Evidence in Medicine
- Jacob Stegenga
“This volume is a collection of philosophy of medicine chapters that deal, in one way or another, with the three linked themes of the title. … The chapters are well-researched and well-written and provide the reader with a useful snapshot of contemporary philosophy of medicine. … this book is a valuable addition to the research literature. ” (Brendan Clarke, Metascience, Vol. 25, 2016)
Editors and Affiliations
Philippe Huneman
Gérard Lambert
Marc Silberstein
Bibliographic Information
Book Title : Classification, Disease and Evidence
Book Subtitle : New Essays in the Philosophy of Medicine
Editors : Philippe Huneman, Gérard Lambert, Marc Silberstein
Series Title : History, Philosophy and Theory of the Life Sciences
DOI : https://doi.org/10.1007/978-94-017-8887-8
Publisher : Springer Dordrecht
eBook Packages : Humanities, Social Sciences and Law , Philosophy and Religion (R0)
Copyright Information : Springer Science+Business Media Dordrecht 2015
Hardcover ISBN : 978-94-017-8886-1 Published: 30 October 2014
Softcover ISBN : 978-94-024-0662-7 Published: 10 September 2016
eBook ISBN : 978-94-017-8887-8 Published: 15 October 2014
Series ISSN : 2211-1948
Series E-ISSN : 2211-1956
Edition Number : 1
Number of Pages : XX, 211
Number of Illustrations : 2 b/w illustrations
Topics : Philosophy of Biology , Theory of Medicine/Bioethics , History of Medicine
- Publish with us
Policies and ethics
- Find a journal
- Track your research
What are 4 types of diseases?

There are many different ways to classify diseases. One common method of classification is by aetiology or the cause of the disease. For example, infectious diseases are caused by pathogens like bacteria and viruses, while chronic diseases are typically the result of lifestyle choices or genetic predisposition. Other classifications include communicable and non-communicable diseases , as well as acute and chronic diseases. Another common method of classification is by pathology or the way in which the disease affects the body. For example, diseases that damage the heart or lungs are typically classified as cardiovascular diseases, while those that damage the nervous system are classified as neurodegenerative diseases.
Regardless of how they are classified, all diseases can have a significant impact on a person’s health and well-being. As such, it is important to be aware of the different types of diseases and how they can affect us. While there are many different types of diseases, these four categories encompass the vast majority of known illnesses: infectious, genetic, metabolic, and external. Read on to learn more.
Infectious diseases
Infectious diseases are caused by microorganisms, such as viruses , bacteria, fungi, or protozoa, that invade the body, attack the immune system and multiply. These pathogens may enter the body through breaks in the skin or the nose or mouth into the respiratory tract. Once inside, if it manages to avoid the body’s immune response it can cause an infection .
Infectious diseases can be spread from person to person through direct contact, such as touching or kissing, bodily fluids, or indirectly through food poisoning by consuming contaminated food containing bacteria such as E. Coli. In some cases, they can also be spread through the air, such as when someone with tuberculosis coughs or sneezes.
Treatment for infectious diseases depends on the type of infection. Some infections, such as the common cold or chickenpox, are mild and go away on their own. Others, such as HIV/AIDS, malaria, or meningitis are more severe and can be life-threatening. Bacterial infections such as the sexually transmitted disease syphilis can be treated with antibiotics, viral infections such as hepatitis B and herpes require antiviral medication while others require more specific treatment. Fungal infections require antifungal medications to treat fungal diseases such as athlete’s foot and ringworm. In some cases, no treatment is available.
Prevention is often the best defence against infectious diseases. Vaccines can help to protect against infections such as the influenza virus, coronavirus, and good hygiene practices can also help to reduce the spread of disease.
Genetic Diseases
There are three main types of genetic disorders: single-gene, chromosome, and multifactorial. Single-gene disorders are caused by a mutation in a single gene. An example of a single-gene disorder is Cystic Fibrosis, which is caused by a mutation in the CFTR gene. Chromosome disorders occur when there is a change in the number or structure of chromosomes. An example of a chromosome disorder is Down syndrome , which is caused by the presence of an extra copy of chromosome 21. Multifactorial disorders are caused by a combination of genetic and environmental factors. An example of a multifactorial disorder is heart disease, which can be caused by a combination of genetic factors, such as family history, and lifestyle choices, such as diet and exercise. Ultimately, all of these different causes can lead to genetic disorders.
Metabolic diseases
Metabolic syndrome is a condition that is characterised by a cluster of health problems that increase the risk of heart disease , stroke, and diabetes. The most common symptoms include high blood pressure , high triglycerides, low HDL cholesterol, high LDL cholesterol, and insulin resistance. If you have three or more of these risk factors, you are considered to have metabolic syndrome. Although the exact cause of metabolic syndrome is unknown, it is thought to be the result of a combination of genetic and lifestyle factors. People who are overweight or obese are at an increased risk for developing the condition, as are those who consume a diet high in processed foods and simple carbohydrates. Treatment for metabolic syndrome typically focuses on lifestyle changes, such as losing weight, eating a healthy diet, and exercising regularly. In some cases, medication may also be necessary to manage individual symptoms.
External diseases
Environmental factors are blamed for causing a variety of diseases. One example is cancer, which can be caused by exposure to harmful chemicals and radiation. Another disease that has been linked to environmental factors is infertility. This is believed to be caused by exposure to chemicals that disrupt the normal functioning of hormones. Other diseases that have been linked to environmental factors include asthma , allergies, and cardiovascular disease. In many cases, it is difficult to identify a single cause of these diseases, as they are likely to be the result of a complex interaction between genetic and environmental factors. However, there is no doubt that the environment plays a significant role in the development of many diseases.
WHO classification of disease
There are many different ways to classify diseases, but one of the most commonly used systems is the International Classification of Diseases (ICD). The ICD is published by the World Health Organization and provides a standard way of classifying both physical and mental disorders. The ICD is regularly updated to reflect advances in medical knowledge, and the most recent version, ICD-11, was released in Feb 2022. The ICD-11 is divided into 21 chapters, each of which covers a different type of disease. For example, Chapter 1 includes infectious diseases such as HIV/AIDS, while Chapter 6 includes mental and behavioural disorders such as schizophrenia . By providing a standard system of classification, the ICD helps countries understand what people get sick from and what eventually kills them. It is used to decide how to plan health services and allocate healthcare spending.
Ultimately, how diseases are classified depends on the particular goal of the classifier. However, all methods of classification offer valuable insights into the nature of diseases and their effects on the human body.
- Health Topics A-Z – CDC
- Health Conditions A to Z
- International Statistical Classification of Diseases and Related Health Problems – WHO
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.
Related Articles

Most common diseases and health risk factors
22 jul 2024.

How can gut health affect your skin and why?
10 nov 2023.

Five signs your bloating is something more serious
16 jul 2024, data security.
Our Commitment to You.

WHY WE BUILT NOWPATIENT
We are committed to helping everyone, everywhere live healthier lives.
The NowPatient virtual care platform provides you with access to trusted health information, affordable treatments, management of chronic health conditions and continuous monitoring for health risks. NowPatient can be accessed by downloading the App or using your web browser.
Download our app today

Your Questions Answered
For your peace of mind, we can answer your questions quickly, what does nowpatient do.
NowPatient is an online pharmacy & telehealth service that is available in the US and UK. Our service is FREE and packed with useful features that can help you save money on the cost of your medications, access virtual treatments, and provide tools that can help improve your overall health.
Get started today and benefit from medication reminders , Get Treated Privately , NHS online pharmacy , GP appointment booking , Rx savings card , Drug Coupons , US drug savings programs , health conditions information , genetic testing , home test kits , BMI Risks , Type 2 Diabetes Risks , pollen meter , air quality monitor , and lots more!
Our service is operated by experienced medical professionals in the United States and the United Kingdom. You can view the online services that we provide by clicking Features .
UK users can safely and securely buy medicines online that treat a wide range of medical conditions. UK customers can also order NHS prescriptions online with the benefit of free tracked delivery.
US customers, regardless of insurance coverage, can enjoy huge savings on prescription medications using our various drug savings programs including drug coupons, savings card and manufacturer-sponsored patient assistance programs.
Where is NowPatient located?
NowPatient has offices in the United Kingdom and United States.
In the UK, we are located at:
NowPatient 28 Chipstead Valley Road Coulsdon Surrey CR52RA
In the US, we are located at:
NowPatient 8911 North Capital of Texas Highway Suite 4200 #1263 78759 Austin, TX
How can I contact NowPatient?
To contact NowPatient, please use the contact form available on the Contact Us page.
Alternatively, if you need to speak to us, you can reach us on the following numbers:
UK telephone number – 020 388 51 500 US telephone number – 1-866-967-1977
Who owns NowPatient?
NowPatient is owned and operated by Infohealth Ltd , a licensed online pharmacy with services spanning the UK, US and Rest of the World. Infohealth Ltd is registered in England and Wales under company number 04004930 and our registered office is at Lynwood House, 373 – 375 Station Road, Harrow, England, HA1 2AW.
Our website is www.nowpatient.com. Our App is called “NowPatient” and can be downloaded from the App Store (for Apple devices) or Google Play (for Android devices).
Can you tell me more about your NHS online pharmacy?
NowPatient’s Pharmaceutical services in the UK are provided by Infohealth Limited trading as ‘Infohealth Pharmacy’.
Our dispensing pharmacy is regulated and authorized for internet sales by the General Pharmaceutical Council (GPhC), registration number 1036487 . You can view our license credentials on the General Pharmaceutical Council website. Our superintendent pharmacist who is responsible for the safe and effective oversight of medicines supplies is Mr Amish Patel (Registration Number 2042705 ).
Medicines are not ordinary items of commerce. All medicines or healthcare product sales are made under the supervision of a registered pharmacist who is licensed by the GPhC. At all times, we endeavour to provide a professional and transparent service whose primary goal is to ensure that the best interests of the patient are served.
How do I make a complaint?
From time to time, we accept that our service levels may not be up to your expectations. NowPatient welcomes concerns, compliments and complaints as valuable feedback that will help us learn from your experiences and make improvements. Feedback can be provided via our clear and transparent Complaints Procedures .
Can you tell me more about NowPatient’s prescribing services for treatments offered?
Our prescribing services are regulated by the General Pharmaceutical Council (GPhC). We provide the following regulated activity:
• treatment of disease, disorder, or injury • transport services, triage, and medical advice are provided remotely • caring for adults over 65 years old • caring for adults under 65 years old
NowPatient prescribing services are run by Infohealth Limited. The Clinical Safety Officer and nominated individual is Mr Navin Khosla .
Can you tell me more about NowPatient’s US services?
Our head of US services is Dr. Jamie Winn .
You can lower the cost of your prescription medications using our various savings programs which include drug coupons, savings card and manufacturer-sponsored patient assistance programs.
We do not provide any prescribing services or dispensing services in the United States.
Is NowPatient legit and can I trust information from NowPatient?
Yes. NowPatient provides trustworthy and accessible clinical, health education and prescription services. We are also trusted by the NHS to deliver clinical and NHS repeat prescription dispensing across the whole of England. In the United States, we work with over 65,000 pharmacies to deliver considerable costs savings for our users.
NowPatient is operated by experienced licensed medical professionals in the United Kingdom and United States. Our Medical Team can be found here.
Our service is trusted by thousands of patients worldwide. You can read their reviews on our Trustpilot:
NowPatient Trustpilot
What are NowPatient’s opening hours?
Our office hours are:
UK – Monday-Friday 9am-6pm GMT US – Monday-Friday 8am-5pm EST
Please note that we are closed at weekends.
In the event of a medical life-threatening emergency please call:
UK – 999 US – 911
In the event of a medical emergency which is not life-threatening please call:
University of Notre Dame
Notre Dame Philosophical Reviews
- Home ›
- Reviews ›
Classification, Disease and Evidence: New Essays in the Philosophy of Medicine

Philippe Huneman, Gérard Lambert, and Marc Silberstein (eds.), Classification, Disease and Evidence: New Essays in the Philosophy of Medicine , Springer, 2015, 211pp., $129.00 (hbk), ISBN 9789401788861.
Reviewed by Robert L. Perlman, University of Chicago
From the Hippocratic Oath to the Nuremberg Code and the Declaration of Helsinki, the philosophy of medicine has been dominated by medical ethics. Recently, however, there has been increased interest in other philosophical issues in medicine, especially in ontological and epistemological questions. Medicine raises the overarching question of the meaning of health and disease, and provides rich case studies that bear on broader issues in the philosophy of science, including causation, reduction, and the mind/body relationship. Moreover, philosophical analyses have important implications for medicine. Clarifying diagnostic categories and methods of diagnosis, and analyzing the evidence for the effects of medical interventions, are ethically significant because they have the potential to improve patient care. As the editors of Classification, Disease and Evidence note, "philosophical topics have direct ethical consequences" (xv).
The book comprises ten essays that present a sampling of recent work in the philosophy of medicine. It is nominally organized around the three concepts in the title, but in the order Disease, Classification, and Evidence. The first four chapters concern the nature of disease and of medicine. Three chapters deal with specific categories of disease -- infectious, psychiatric, and genetic -- motivated by the understanding that classification is an essential part of diagnosis. We want to know not just what disease a patient has but what kind of disease he or she has. Indeed, medicine is organized around specific classes of disease. Finally, three chapters deal with issues of evidence, or epistemology. How do we know what we think we know? What evidence is needed to provide reliable knowledge and to justify or rationalize medical decisions?
In "Objectivity, Scientificity, and the Dualist Epistemology of Medicine," Thomas V. Cunningham challenges the conventional view that medicine is both "science" and "art." Cunningham argues that the domain that has commonly been considered the art of medicine -- physicians' modes of communication, their knowledge of patients' histories, values and preferences, and the integration of this understanding into patient care -- is amenable to objective analysis under the rubric of clinical decision science, and so is also scientific. Moreover, Cunningham points out that recent philosophy of science has criticized the notions that science is value-free and that it is concerned only with general laws and not with particular phenomena. Cunningham concludes, "clinical medicine should be understood as an integrative science that draws on various methods, which are objective by varying degrees" (8), and "the popular philosophical distinction between the art and science of medicine ought to be rejected and in its place a unified multifaceted epistemology of medicine should be developed" (15). Whether it is better to think of medicine as a multi-faceted science than as a combination of science and art is questionable, but it is useful to be reminded that all aspects of medicine can be studied empirically and that knowledge gained from these different approaches needs to be integrated to optimize patient care.
Several contemporary philosophers, most notably Christopher Boorse and Jerome Wakefield, have proposed general theories of disease. Their proposals, which use concepts of normal function and dysfunction to distinguish between health and disease, have met with only limited acceptance. In "The Naturalization of the Concept of Disease," Maël Lemoine argues that we should focus on disease explanations, or disease mechanisms, rather than on judgments as to what is or is not a disease. Considering diseases in terms of their pathophysiological mechanisms, a methodology Lemoine calls naturalization, may allow a general theory of disease that has eluded conceptual analyses of the differences between disease and non-disease. Lemoine is optimistic that network medicine, the study of networks of connectivity between genes and environmental factors that are implicated in disease, or the closely related field of systems biology, will provide a framework for a general theory of disease. Grounding the philosophy of medicine in our best current understanding of human biology is certainly a good idea, but it isn't yet clear that either network medicine or systems biology will be able to do what Lemoine hopes they will.
Several chapters deal with psychiatry and mental disorders. Dominic Murphy's "What Will Psychiatry Become?" concerns the causal structure of mental illness. In the first part of his essay, Murphy makes the important distinction between reduction and levels. While psychiatry should strive to reduce mental illnesses to their causes, this does not necessarily entail reducing them to lower structural or functional levels. Thus, both genetics and unemployment may be causes of depression. Murphy goes on to consider psychiatry as a branch of cognitive neuroscience. In his view, "classification and causal explanation [of mental illness] will be ultimately founded on the neurophysiological organization of the mind" (47). In this process, neurobiological concepts will replace outmoded psychological concepts such as beliefs and desires. Murphy uses addiction to illustrate how psychiatric problems can be understood in terms of neuroscience. We can discuss addiction with reference to dopaminergic circuits and the like, and provide a causal model in terms of neurochemistry without need of psychological concepts. But addiction may not be a good model for all psychiatric disorders. And Murphy's analysis leads him to end on a somber note: "Psychiatrists will always need to be able to help people understand what they have become. The worry is that greater understanding of the mind will make it harder for us to explain people to themselves" (60).
Both Boorse and Wakefield discuss psychiatric illnesses, like other illnesses, as disorders of function. In "The Function Debate and the Concept of Mental Disorder" Steeves Demazeux considers the value of these approaches for psychiatry. Demazeux agrees with Boorse and Wakefield that mental diseases should be analyzed as a subset of disease in general, and that psychiatry is a legitimate branch of medicine. He argues, however, that there are flaws in both Boorse's and Wakefield's analyses, and that neither provide a valid framework for understanding mental disorders. It is difficult to identify individual mental functions or to develop objective criteria for distinguishing normal from pathological. Wakefield adopts an essentialist view of disease, and neither he nor Boorse takes sufficient account of variation among patients or of the natural history of disease. Deciding when in the course of a psychiatric or other medical problem a dysfunction should be considered a disease is a subjective matter. Demazeux ends by suggesting that we should consider individual psychiatric disorders separately and should be prepared to conclude that some may be considered mental diseases and others not.
The editors emphasize evolution and the new field of evolutionary medicine (or evolutionary medicine and public health, as it is now being called) in their introduction. Only one chapter, however, "Emerging Disease and the Evolution of Virulence: The Case of the 1918-1919 Influenza Pandemic" by Pierre-Olivier Méthot and Samuel Alizon, is explicitly concerned with evolution and medicine. Evolution is a two-step process, comprising variation (mutation) and selection. Since the rediscovery of Mendel's Laws at the beginning of the twentieth century, there has been a tension between the research programs that have emphasized one or the other of these two processes. Méthot and Alizon have used the 1918-1919 influenza pandemic as a case study to show how this tension continues to play out in our understanding of the evolution of virulence. One school of research seeks to find virulence factors, individual genes or suites of genes that increase the virulence of pathogens. Molecular biologists and geneticists have reconstructed the complete genomic sequence of the 1918-1919 pandemic influenza strain in an effort to determine the molecular causes of the high virulence of this strain. Another school focuses on the ecological factors that lead to the spread of more virulent pathogens. Ecologists have pointed to the crowding, poor nutrition, and poor health of troops at the front line of World War I, together with the transport of wounded soldiers to military hospitals, as creating the conditions that would select for increased virulence. While both approaches have yielded valuable information, neither by itself has explained the high virulence of this virus. Méthot and Alizon emphasize how the molecular and ecological research programs have been pursued independently, with little interaction, and sensibly call for an integration of these approaches to understanding the evolution of virulence. As we pay increasing attention to emerging infectious diseases, it will be important for physicians and biomedical scientists to heed this advice.
In "Power, Knowledge, and Laughter: Forensic Psychiatry and the Misuse of the DSM ," Patrick Singy uses paraphilias as a case study to discuss the relationship between psychiatry and the law. In the first part of his chapter, Singy questions the objectivity of psychiatric diagnoses, pointing out, for example, that homosexuality used to be considered a mental disorder. He goes on to argue that even if psychiatric diagnoses were objective, psychiatry and the legal system are concerned with two different problems. Forensic psychiatrists are interested in whether or not a defendant has a mental illness, while the legal system must determine a defendant's capacity or incapacity to control his or her actions. Although mental diseases and incapacities are overlapping categories, they are not identical and are logically distinct. Singy claims that some people who are diagnosed with a paraphilia have the capacity to regulate their behavior and some do not. For this reason, he argues that psychiatric testimony about the presence or absence of a paraphilia or other mental disease has no place in the courtroom. In his view, psychiatry will enhance its legitimacy if it doesn't overstep its proper functions, and the law will be administered more fairly if it isn't distracted by psychiatric diagnoses.
"Defining Genetic Disease," by Catherine Dekeuwer, is the only chapter that is really concerned with the classification of diseases. Defining genetic disease turns out to be more complex than we might have thought. There is probably genetic variation in susceptibility to virtually all diseases. We study genetic risk factors because they may give insights into disease pathogenesis and into ways of manipulating the environment to prevent or ameliorate disease. Dekeuwer suggests that we define genetic disease as "a hereditary disease whose fundamental (molecular) defect has been identified at the level of DNA. This defect explains the disease's characteristics on higher levels (cellular, tissue, physiological)" (155). While this definition may express a laudable research goal, it does not accord with either the historic or the contemporary use of the term "genetic disease" in medicine. Long before genes were identified as DNA sequences, genetic diseases were defined as diseases that were inherited in a Mendelian fashion. Even today, when many "disease genes" have been cloned and sequenced, we often cannot explain disease phenotypes in terms of the absent or altered biological activities of the proteins that these genes specify. Genetic diseases are commonly recognized as hereditary diseases caused by alleles with a high level of penetrance or a flat norm of reaction, such that all or most of the people who inherit these alleles develop the disease. Again, however, there is no clear demarcation between genetic diseases and diseases for which there are genetic risk factors. Dekeuwer cautions against expanding the definition of genetic disease because of the common if unwarranted tendency to conflate "genetic" with "inevitable." She fears that our focus on genetic determinants of disease may reinforce folk notions of the geneticization of people and of human behavior.
In "Causal and Probabilistic Inferences in Diagnostic Reasoning: Historical Insight into the Contemporary Debate," Joël Coste highlights the different kinds of evidence and inferences that physicians use in making diagnoses. Causal reasoning is most applicable to genetic and infectious diseases. If physicians find specific genes or pathogens, they reason that these are the causes of disease, and make diagnoses accordingly. This kind of reasoning does not require knowledge or consideration of the pathophysiological mechanisms that intervene between the causes and the manifestations of disease. As noted above, we often do not understand how mutant alleles cause specific diseases. Physicians use pathophysiological reasoning for many neurological diseases, where they can determine the site of lesions from the pathophysiology even if they don't know the cause of these lesions, and in endocrinology, where analysis of feedback mechanisms can give insights into the seat of disease (hypothalamic, pituitary, or peripheral endocrine gland), again often without knowledge of the cause of the disease. Still other diseases are defined and diagnosed on the basis of their symptoms, even if neither the cause nor the pathophysiology of the disease is known. Coste contrasts this causal reasoning with what he calls probabilistic or empirical approaches to diagnosis, and notes the longstanding tension between deterministic and empirical approaches to diagnosis, or to medicine more broadly. Coste's conclusion, that this tension between the desire to explain and the desire to be effective is inherent to medicine, echoes Murphy's concern that the explanation of mental diseases in neurobiological terms may impede psychiatry's effectiveness.
"Risk Factor and Causality in Epidemiology," by Élodie Giroux, addresses the vexed problem of the relationship between risk factors and causality, or between risk factors and disease. The Framingham Heart Study, one of the major epidemiological studies of cardiovascular disease, identified risk factors for coronary heart disease but could provide little evidence that these risk factors were causal. At about the same time, studies of the association of cigarette smoking and lung cancer led to the argument that smoking was not just a risk factor for lung cancer but was actually causal. Bradford Hill developed criteria for making causal inferences from risk factor associations. With smoking and lung cancer, the evidence was overwhelming and the analysis relatively straightforward. The causal status of many other risk factors, however, has been open to debate. Some philosophers have advocated a probabilistic concept of cause, such that "a risk factor is considered causal because it increases the probability of its effect" (187). Many epidemiologists, however, have argued that causes must be analyzed in terms of their sufficiency and necessity, and the mechanistic connections between causes and effects. These differing views of the relationship between risk factors and causes have led to what Giroux refers to as "a tension between mechanistic considerations and statistical or probabilistic considerations" (188). Analyzing and resolving this tension remains a major challenge for philosophers of science. Giroux concludes by highlighting "the important part that epidemiology plays in the development of criteria for causal inference" (190).
Evidence-based medicine is governed by a hierarchy of evidence according to which systematic reviews or meta-analyses of randomized, controlled clinical trials are at the top of the hierarchy and anecdotal observations are at the bottom. Despite many criticisms of this hierarchy, it remains the prevailing way of evaluating evidence to guide medical interventions. In "Herding QATs: Quality Assessment Tools for Evidence in Medicine," Jacob Stegenga raises other difficult problems with evidence hierarchies. He points out that clinical trials have many elements -- randomization, blinding (or masking), placebo or other controls, withdrawals or dropouts, etc. In comparing studies, how does one weight these various elements? Many authors have developed what Stegenga refers to as Quality Assessment Tools, or QATs. Because these different QATs assign different weights to the various components of clinical trials, there is poor inter-tool reliability. Although Stegenga believes that QATs should replace hierarchies in the assessment of evidence, there is as yet no theoretical or empirical way of assessing the QATs themselves. Whether QATs will replace or supplement evidence hierarchies remains to be seen, but as Stegenga shows, not only may the available evidence underdetermine appropriate medical decision-making, but the quality of the evidence itself is underdetermined. Evidence-based medicine is directly concerned with improving patient care, and so the development of better ways of assessing evidence is one of the philosophy of medicine's most important ethical projects.
The essays in this collection are interesting, opinionated, and provocative. They express original, personal views rather than the conventional wisdom on the subjects they discuss. Even when the authors' arguments are not convincing, they are thought provoking and worth considering. Unfortunately, the book itself is poorly edited and does not add much value to the individual contributions. Several topics, including general theories of disease and the nature of mental illness, are discussed in more than one chapter, but with the exception of one footnote the authors make no reference to one another, and without an index it is difficult for readers to relate the various arguments of the different authors. Four of the essays were initially published in French. The editors do not identify the translator(s) of these chapters. And as one other annoying example of poor editing, different authors use different citation formats. The intended audience for this collection isn't clear. While many readers will be interested in one or several chapters, I suspect that few will want to read the whole book.
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Why the communicable/non-communicable disease dichotomy is problematic for public health control strategies: implications of multimorbidity for health systems in an era of health transition
Nigel unwin.
- Author information
- Article notes
- Copyright and License information
Corresponding author: Present address: Room 4.41 Falmouth Building, Faculty of Health Sciences, University of Cape Town, Anzio Road, Observatory 7925, Cape Town, South Africa; E-mail: [email protected]
Received 2015 Feb 9; Revised 2015 Apr 23; Accepted 2015 May 5; Issue date 2015 Nov.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License ( http://creativecommons.org/licenses/by-nc/4.0/ ), which permits non-commercial re-use, distribution, and reproduction in any medium, provided the original work is properly cited. For commercial re-use, please contact [email protected]
In today's globalized world, rapid urbanization, mechanization of the rural economy, and the activities of trans-national food, drink and tobacco corporations are associated with behavioral changes that increase the risk of chronic non-communicable diseases (NCDs). These changes include less healthy diet, lower physical activity, tobacco smoking and increased alcohol consumption. As a result, population health profiles are rapidly changing. For example, the global burden of type 2 diabetes mellitus is expected to double by 2030, with 80% of adult cases occurring in low and middle-income countries (LMIC). Many LMIC are undergoing rapid changes associated with developing high rates of NCD while concomitantly battling high levels of certain communicable diseases, including HIV, TB and malaria. This has population health, health systems and economic implications for these countries. This critical review synthesizes evidence on the overlap and interactions between established communicable and emerging NCD epidemics in LMIC. The review focuses on HIV, TB and malaria and explores the disease-specific interactions with prevalent NCDs in LMIC including diabetes, cardiovascular disease, chronic obstructive pulmonary disease, chronic renal disease, epilepsy and neurocognitive diseases. We highlight the complexity, bi-directionality and heterogeneity of these interactions and discuss the implications for health systems.
Keywords: Co-morbidity, Communicable disease, Health transition, Infectious disease, Low and middle-income countries, Non-communicable disease
Introduction
The broad classification of diseases into communicable (infectious) and non-communicable diseases (NCDs) is deeply ingrained. However, this classification may be unhelpful for setting public health priorities, particularly in low- and middle-income countries (LMIC). 1 For example, using data from Tanzania it has been shown that classifying diseases as acute versus chronic, rather than communicable versus non-communicable, dramatically changes the distribution of disease burden. 2 The ‘acute versus chronic’ approach to disease classification demonstrated the equal burden of diseases requiring chronic care versus acute care even though the vast majority of the disease burden was classified as ‘communicable’. 2
We focus on interactions likely to be of public health importance in LMIC, but also in marginalized populations in high-income countries. We argue that public health approaches to the prevention and control of these diseases must be fully informed by these interactions and move beyond the communicable/non-communicable divide.
The context of the epidemiologic transition
On a superficial level the original concept of the epidemiologic transition 3 can appear to provide a clear rationale for the communicable/non-communicable divide. The transition is seen to consist of falling mortality from communicable diseases, particularly in infancy and childhood, followed by an increasing predominance of deaths from ‘man-made degenerative diseases’. 3 However, this was always a limited interpretation. Re-analysis of historical data from Sweden has shown how patterns of falling death rates varied greatly between different regions, with some continuing to experience high rates of communicable disease mortality while this fell dramatically in others. 4 It is clear that over the past 50 years many low and middle-income countries have seen emerging epidemics of chronic NCDs while continuing to experience high rates of communicable disease. 5
Table 1 illustrates the heterogeneity of conditions contributing to the burden of disease in 12 low and middle-income regions. It highlights the significant contribution of NCDs to disability-adjusted life years lost in most LMIC. In eight of the regions, including Southern Africa, North Africa/Middle East and Latin America, both major communicable diseases and NCDs are within the top 10 conditions contributing to the burden of disease. This highlights the fact that a continued approach to public health along the dichotomous parallel lines of communicable and NCDs is increasingly redundant in these settings. Interactions between communicable and NCDs are complex and often mediated by shared risk factors (Figure 1 ). This critical review aims to provide an up to date account of interactions between, and co-existence of, NCDs and communicable diseases that lead to increased morbidity and are likely to be of public health importance to LMIC, as well as marginalized populations in high-income settings.
Rankings of diseases according to their contribution to disability adjusted life years (DALYs) in different global regions
COPD: chronic obstructive pulmonary disease.
Adapted from Murray CJ, Vos T, Lozano R et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2197–223.
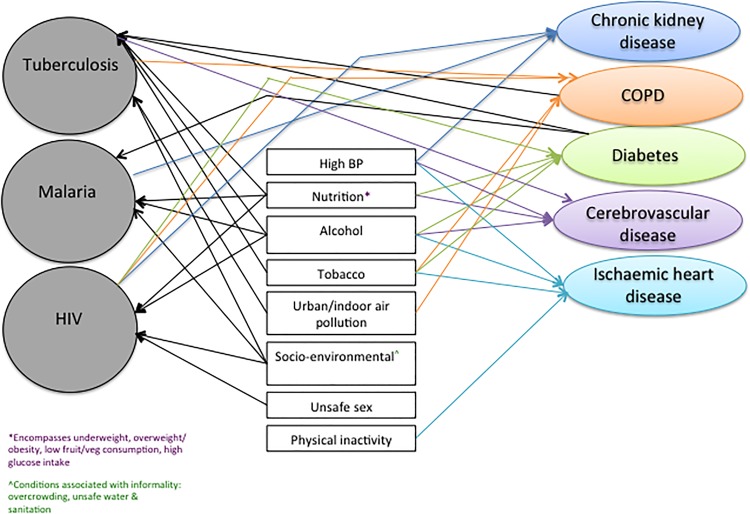
Interaction between TB, Malaria and HIV, and risk factors/disease precursors and non-communicable diseases. BP: blood pressure; COPD: chronic obstructive pulmonary disease. This figure is available in black and white in print and in color at International Health online.
The literature search was carried out between October 2013 and December 2014 and included literature published until December 2014. Our aim was to conduct a ‘critical review’. 6 Unlike a systematic review, this does not aim at a comprehensive assessment of original research but rather seeks to identify the conceptual contribution of existing literature to the field of study. 6 We searched for literature (English language) using the PubMed and EMBASE databases and the following combination terms (as MESH terms and key words): (HIV OR tuberculosis OR malaria) AND (diabetes mellitus OR chronic obstructive pulmonary disease OR chronic kidney disease OR cardiovascular disease OR cardiomyopathy OR metabolic syndrome OR neurocognitive disease OR dementia OR epilepsy). From the 24 864 articles identified by this search strategy, we honed down on original research and review articles with titles and abstracts that were clearly pertinent to co-morbidity and interactions between one or more of the three communicable diseases and NCDs. Articles were selected to ensure comprehensive representation of interactions reported in the literature. Both authors identified and reviewed papers and 80 articles were eventually included in the review. Of note, there was a lot of information about the NCDs and TB or HIV interactions but far fewer studies on malaria and NCDs.
Tuberculosis
As Table 1 shows, TB remains a leading cause of disability-adjusted life years in many regions of the world, particularly in poor populations in LMIC. In 2012 it is estimated that there were 8.6 million new cases and 1.3 million deaths from TB. 7 Tuberculosis is preventable and curable, and therefore the goal of much lower incidence and mortality is appropriate. 8 In 2014 the World Health Assembly adopted ambitious new targets for TB: a 90% reduction in incidence and a 95% reduction in the number of deaths between 2015 and 2035. 9 Achieving a 90% reduction in incidence by 2035 will require a marked improvement in the rate of decline, from around 2% per year at present, to 10% per year by 2025. 8 Achieving a 95% decrease in mortality will require more than halving the case fatality from 15% to 6.5% by 2025. 8 Tackling this challenge will require improvements in diagnostic and treatment services and identification and reduction of risk factors that increase TB susceptibility. Diseases and risk factors that impair immune function, such as malnutrition, alcoholism or HIV co-infection, can increase the likelihood of infection or reactivation of latent TB. A study of the effect of multiple exposures to these risk factors reported that tobacco use, alcohol, type 2 diabetes mellitus (T2DM) and low body mass index (BMI) were significant individual risk factors and associated with triple or quadruple the risk of TB with multiple exposures. 10
Tuberculosis and diabetes
Type 2 diabetes mellitus is a risk factor for TB. Two systematic reviews have demonstrated that T2DM increases the risk of incident TB by around threefold. 11 , 12 Together these reviews included 15 studies, the vast majority of which were from high-income countries. Since they were published more data have accumulated from low and middle-income settings, essentially confirming the increased risk of TB in people with diabetes. 13 In a case control study from Tanzania, for example, diabetes was associated with fourfold increased risk of TB in HIV negative, but not positive, patients 14 Because diabetes is common (affecting 8.3% of the global adult population, based on International Diabetes Federation estimates for 2014 8 ) the number of cases of TB attributable to diabetes is large. Globally, for example, diabetes is estimated to account for 15% of all adult cases of TB. Even in Africa, where diabetes prevalence in adults is estimated to be 5% (the lowest of all regions), and HIV is a major contributor to TB incidence, diabetes is still thought to account for almost 1 in 10 adult cases. 8
In addition to increasing the risk of incident TB, diabetes is also a risk factor for poorer TB outcomes. A systematic review and meta-analysis found that the risk of death during TB treatment was almost twice as high in those with diabetes compared to those without, and relapse following treatment almost four times as high. 15
These interactions between diabetes and TB have implications for achieving the 2035 WHO targets for TB incidence and mortality. 9 Diabetes prevalence is expected to continue to increase over the coming decades, especially in LMIC. 16 Conservative estimates suggest that it will increase to around 10% globally in adults in 2035 16 and the results of modelling suggest that this would offset the present downward trend in incidence by around 3%. 8 A less conservative estimate of the increase in diabetes prevalence, suggests that it will be 13% in 2035 and this would offset the decline in TB incidence by 8%. 8
The strong association between TB and diabetes, and the poorer health outcomes associated with their co-existence, naturally leads to the question of whether patients with one condition should be screened for the other. The latest WHO strategy 9 recommends screening people with diabetes for active TB in settings with a high TB burden, such as where the TB incidence is 100 cases per 100 000 persons/year or more. The type of screening will depend on resources. A practical approach described in China and India is to screen all people with diabetes on each clinic visit with a symptom-based questionnaire with referral for further investigations for those who are positive. 8 The WHO strategy also recommends that all people with TB are screened for diabetes, with referral for diabetes diagnosis and management for those who are positive. 9
It is clear that diabetes and TB are intimately related. However, there remain many unanswered questions as to the most effective approaches to minimizing the morbidity and mortality from this interaction. These were summarized in a recent review 13 and include the following: what is the effect of glycaemic control on new TB infection, active TB and TB treatment outcomes, and what are the most effective approaches to achieving glycaemic control in people with TB? what are the most feasible and valid approaches to screening for diabetes in patients with TB (noting that inflammation from TB infection may cause a transitory hyperglycaemic response)? what models of health care delivery can deliver sustainable, integrated and cost-effective care for diabetes and TB in LMIC? and is screening and prophylactic treatment of latent TB infection indicated in people with diabetes?
A significant contribution to answering some of the questions on the diagnosis of diabetes in TB, the role of glycaemic control on TB outcomes, and the best way to deliver care, is being made by the TANDEM study, 17 which began in 2013. This is a study working in four endemic TB countries that are experiencing rapid rises in diabetes prevalence (Romania, Peru, South Africa and Indonesia) and supported by researchers in Germany, UK and the Netherlands.
Tuberculosis and chronic obstructive pulmonary disease
Figure 1 shows the bi-directional nature of the interaction between TB and chronic obstructive pulmonary disease (COPD). Due to the similarity between TB and COPD symptoms, there is potential for missing the diagnosis of one when they co-exist. Persons with COPD have been found in one study to have a two to threefold higher risk of developing TB, 18 and a twofold increased mortality compared to non-COPD patients. 19 The increased risk of TB associated with COPD is often attributed to smoking. 20 However, studies have also found an association between oral corticosteroid use in COPD patients and TB risk. 18 A systematic review confirmed that although this association is independent of smoking, 21 the risk of COPD is further increased by tobacco smoking and low socioeconomic status, common risk factors for both COPD and TB.
The histopathological changes that occur in the lungs of TB patients can result in anatomical changes associated with both obstructive and restrictive patterns of impaired lung function of varying severity, which can persist after successful completion of TB treatment. 22 The prevalence of COPD after TB treatment completion varies from 28 to 68%, 23 and is further increased in persons with multiple episodes of TB. 24 Childhood studies have also demonstrated this association, due to prolonged bronchial obstruction by enlarged lymph nodes during TB disease. 25 In LMIC, alongside a concomitant rise in the prevalence of tobacco smoking, TB is an important contributor to poor quality of life and disability-adjusted life years lost due to COPD. 26 A study in South Africa reported that the strongest predictor of chronic bronchitis was a history of TB. 27 Early identification and management of chronic lung impairment is therefore crucial to minimizing the long-term negative impact of TB.
Tuberculosis and chronic kidney disease
The prevalence of chronic kidney disease (CKD) is increasing, and it is estimated that 70% of patients with end stage renal disease will reside in LMIC by 2030. 28 This has significant implications on infrastructural and financial resources. The most common causes of CKD in LMIC are chronic glomerulonephritis and interstitial nephritis due to infections, including TB. 28 Conversely, patients with CKD and patients on dialysis are at an increased risk of TB and poorer TB outcomes. 29 One study in India reported a 4% incidence of TB, despite negative tuberculin skin tests (TST) in the majority. 30 Similarly, a study of hemodialysis patients in Turkey also reported a 3.1% incidence of TB with almost 40% of patients having a negative TST. 31 This suggests that there should be a high index of suspicion of TB in these patients regardless of TST results. Examining factors associated with treatment non-adherence or death, a study in Brazil found that socio-demographic characteristics such as younger age and alcoholism were associated with poorer outcomes. 32
The co-existence of TB also complicates management of blood pressure in CKD patients, as concurrent TB treatment is associated with a decrease in the potency of antihypertensive treatment. 33
Tuberculosis and the heart
Tuberculosis is the most common cause of pericarditis in Africa and other high TB burden settings, often presenting with symptoms similar to those of heart failure. 34 The increase in the burden of TB pericarditis has been attributed to HIV 35 and in the Western Cape, South Africa, 50% of patients with pericardial effusions have HIV. 36 Given these data, TB is an important consideration in persons presenting with heart failure in high TB burden settings, especially if HIV-infection is present. However, significant challenges remain, including diagnostic difficulty due to atypical presentation and varying evidence on the optimal management of these co-morbid conditions. 35
Globally, HIV is the fifth and sixth leading cause of DALYs lost and mortality, respectively. 37 , 38 There are promising signs that the HIV pandemic is abating in high burden settings, with declining incidence and mortality rates. 39 Nonetheless, the rising NCD morbidity and mortality rates alongside an established HIV epidemic make it crucial to better understand the interactions that exist with emerging NCD and disease precursors, both related to HIV directly or as a side effect of antiretroviral therapy (ART). LMIC bear a disproportionate burden of the HIV pandemic. Furthermore, HIV-infected adults on treatment have higher than expected risk of several non-AIDS disorders, including cardiovascular disease and kidney disease in addition to adverse effects associated with ART. 40 , 41 HIV has also been identified in a case control study as an independent risk factor for stroke in urban and rural Tanzania, 42 although there is a paucity of data on the nature and extent of this interaction in LMIC.
HIV and metabolic syndrome
There is conflicting evidence on an association between HIV infection and hyperglycemia (including T2DM) independent of ART. 43 , 44 The use of ART containing protease inhibitors (PI) and nucleoside reverse transcriptase inhibitors has been associated with insulin resistance. 45 , 46 A Cape Town survey of HIV-infected persons on ART reported a 21.9% prevalence of newly detected hyperglycemia and a significant association with efavirenz (a non-nucleoside reverse transcriptase inhibitor). 47 HIV-related dyslipidemia independent of ART has been described. 48 The use of ART is also associated with dyslipidemia, peripheral wasting and central fat accumulation. In particular PI and non-nucleoside reverse transcriptase inhibitors (NNRTI)-based regimens have been associated with dyslipidemia and atrophy. Protease inhibitor drugs are particularly associated with dyslipidemia, a known risk factor for cardiovascular complications 49 , 50 ; patients with baseline elevated lipid levels have the greatest risk of developing dyslipidemia, especially hypertriglyceridemia. 49 A study conducted in South Africa reported an association between ART and increased central fat and reduced peripheral fat; partially improved by switching from an NNRTI to a PI-based regimen. 51
HIV and the heart
The most commonly reported cardiac manifestation in HIV is pericardial disease, often due to TB. 52 HIV-related dilated cardiomyopathy is also common with the prevalence in the pre-ART era ranging between 18 and 43% in LMIC. 53 , 54 The prognosis of this condition has historically been poor, 55 , 56 although the prevalence has decreased with the roll out of ART. 52 Evidence from Africa on the prevalence of echocardiographic abnormalities in asymptomatic persons with HIV is limited although documented in other regions to vary from a 34–48% prevalence of systolic and diastolic dysfunction, and >10% prevalence of dilated cardiomyopathy. 57 , 58 Pulmonary hypertension is also associated with HIV infection, with a prevalence of between 0.5 and 5%. 52 Although mortality associated with pulmonary hypertension has significantly decreased post-ART roll out, specific treatment for pulmonary hypertension is required to improve cardiac function. 59 There is an increased risk of myocardial infarction in patients with HIV on ART, particularly in patients with metabolic syndrome. 60 Protease inhibitor drugs have been shown to be associated with a 26% increase in the rate of myocardial infarction per year of exposure, partially due to dyslipidemia. 61 This was found with some (e.g., indinavir, ritonavir-boosted lopinavir 62 ) but not others (boosted atazanavir 63 ). Evidence on the cardiovascular disease (CVD) risk associated with nucleoside reverse transcriptase inhibitors is conflicting; however a recent meta-analysis demonstrated no increased risk. 64 There has been no proven association between T2DM and other ART drug classes. Drug-drug interactions are also important to mention due to interaction of ART with the cytochrome P450 pathway. 52
HIV and chronic kidney disease
Chronic kidney disease is an important cause of morbidity and mortality in persons with HIV, including HIV-associated nephropathy and membranoproliferative glomerulonephritis, particularly in hepatitis C co-infection. 65 The risk of CKD is further increased in the presence of other risk factors including older age, hypertension, diabetes, and black ethnicity. 66 Although the incidence of CKD has been remarkably altered by widespread ART access, some ART regimens are associated with incident acute or chronic kidney disease. 67 Studies of HIV-infected patients on ART in Taiwan and Vietnam reported a 7% prevalence of CKD, with older age, lower body weight and tenofovir use being independently associated with CKD. 68 , 69 However, the benefits of tenofovir are considered to outweigh the nephrotoxic side effects. 70
HIV and chronic obstructive pulmonary disease
Studies have shown an increased risk of COPD in HIV-infected patients. Studies conducted in the pre-ART era demonstrated an association between HIV and airway hyper-responsiveness as well as radiographic emphysema. 71 , 72 A post-ART era study conducted in the USA showed that after adjusting for known COPD risk factors, HIV remained an independent risk factor for COPD with patients with HIV 50–60% more likely to have COPD than HIV-negative. 73 These findings have been confirmed in other studies conducted in the USA 24 , 74 and Italy. 75 A French study reported a 26% prevalence of COPD among persons with HIV, 74% of which were previously undiagnosed. 76 There is a paucity of data on HIV and COPD from high HIV prevalence LMIC. With increasing periods on ART, pulmonary complications are shifting from opportunistic infections to non-infectious complications such as COPD.
HIV and the brain
Neurocognitive disease and dementia.
We highlight three aspects of ageing in HIV: patients with HIV are surviving for longer periods; an increasing proportion of incident HIV cases are in older persons who may perceive themselves to be at low risk of HIV; and HIV and ART are thought to be associated with acceleration of the ageing process such that illnesses associated with advanced age occur at younger ages. 77 These combined processes mean that co-morbidity of neurocognitive disorders such as HIV-associated neurocognitive disorder (HAND) will become increasingly more common. A study in Nigeria reported a 21.5% prevalence of HAND in HIV-infected patients on ART for at least 1 year. 78
Epilepsy and seizures
Seizures, a neurological manifestation of HIV infection, are mostly of the generalized type, and are more common in advanced stages of HIV, although they may rarely be the presenting manifestation or occur early in the course of illness. 79 Reported causes include mass lesions, opportunistic infections including toxoplasmosis and cryptococcal meningitis and the direct effect of HIV on the brain (HIV encephalopathy). 79 The reported incidence of new-onset seizures varies from 4–20% 79 , 80 with a higher prevalence in LMIC, likely due to a higher prevalence of opportunistic infections. The management of co-morbid HIV and epilepsy can be challenging. Phenytoin is the most commonly prescribed anti-epileptic drug and this drug induces the CYP450 system and can result in ART failure to control HIV viral replication 81 or phenytoin toxicity. 82 This highlights the importance of careful monitoring of viral load and anti-epileptic drug levels, and careful selection of anti-epileptics such as levetiracetam. 83 However, in many LMIC, choices of anti-epileptic drugs are limited.
Malaria is a parasitic infection that is responsible for at least half a million deaths per year (estimated to be 660 000 in 2010, uncertainty range from 490 000 to 836 000), and around 200 million clinical cases per year (219 million in 2010, uncertainty range 154 to 289). 84 Eighty percent of all deaths occur in just 14 countries, with 40% occurring in just two: Nigeria and the Democratic Republic of the Congo. 84
Malaria is caused by the protozoan Plasmodium , which is transmitted between humans by the Anopheles mosquito. There are four species of Plasmodium causing disease in humans, of which vivax and falciparum are the most common; falciparum is the most deadly because of its tendency to involve the brain (cerebral malaria). Roughly 30% of the world's population lives in areas where there is a risk of falciparum malaria. 85 Groups at high risk of severe and life threatening infection are those with no immunity (e.g., children, and visitors from non-endemic areas) and with impaired immunity (e.g., those with HIV/AIDS). However, immunity is relatively short lived and those returning to endemic areas after several months or years are also at increased risk because of reduced or absent immunity. 84
Malaria is, of course, associated with the environmental conditions that favour the breeding of its mosquito vector. However, similar to the major NCDs it is also associated with poor socio-economic conditions, and it has been suggested that economic development per se will reduce its impact. 86 Other shared risk factors with NCDs are less clear. The relationship between poor childhood nutrition, a risk factor for T2DM and cardiovascular disease, and the risk of malaria is unclear. 87 – 90
Malaria and diabetes
There is evidence from a recent case control study conducted in urban Ghana that people with T2DM are roughly 50% more likely to show evidence, based on testing for the DNA of the parasite, of infection with falciparum malaria. 91 It is important to note that participants in this study did not have clinical malaria. However, the findings do support the hypothesis that people with T2DM may be at increased risk of clinical malaria.
Clinical malaria in adults with T2DM is likely to be relatively common in endemic areas that also have a high prevalence of T2DM, such as many urban centers in Africa and Asia. However, there is a lack of evidence on whether people with T2DM who develop clinical malaria have poorer outcomes than people without T2DM.
Malaria and chronic kidney disease
Chronic kidney disease and risk of malaria.
Chronic kidney disease was ranked the 18th commonest cause of death globally in 2010, estimated to have caused 736 000 deaths. 92 Type 2 diabetes mellitus and hypertension are the two most important risk factors for CKD, 92 and as these increase in LMIC, so will CKD. The clinical end point of CKD is end stage kidney disease, which can be defined by the requirement for life saving dialysis or renal transplantation. 93 Worldwide it is estimated that 1.9 million people are undergoing some form of renal replacement therapy. 94 In LMIC, it is estimated that only around a quarter of those who require renal replacement therapy receive it.
It is not known if CKD increases the risk of clinical malaria. It is known, however, that renal transplantation in malarial areas is associated with a risk of malaria in the recipients, the infection being transmitted via the donor kidney. 95 Thus, it is recommended that renal transplant patients in malarial areas receive appropriate prophylaxis to eliminate the risk of this potentially life threatening complication. 95
Finally, three of the drugs commonly used in malaria prophylaxis (malarone, proguanil and chloroquine) may be contraindicated in patients with CKD, depending on the level of renal impairment. 96
Malaria as a cause of kidney disease
One form of malaria, caused by Plasmodium malariae , is associated with a risk of progressive renal damage (nephrotic syndrome) which even after successful eradication of the infection may progress to end stage kidney disease, and thus require renal replacement therapy. 95 This condition occurs predominantly in children and young adults. While it is a well-recognized condition, good estimates of its incidence and overall contribution to end stage kidney disease are lacking. It is thought to occur in only a fraction of Plasmodium malariae infections but it is described as one of the major causes of renal disease in children living in malarial areas. 97
It is estimated that falciparum malaria is associated with acute renal failure in 1–5% of cases occurring in local inhabitants in endemic areas, but that in non-immune visitors around a quarter suffer this complication. 95 Successful treatment of the infection normally leads to recovery of renal function within 2–6 weeks. However, during the acute phase many patients (40–70%) require dialysis. 95
Discussion of implications for health systems
This review highlights the complex interactions between established communicable and emerging NCDs in LMIC. The results emphasize the importance of re-thinking disease classifications in the context of disease prevention, promotion, treatment and care.
The increasing prevalence of communicable/NCD multimorbidity in many LMIC settings, particularly in socio-economically disadvantaged groups suggests that this changing pattern of disease has significant implications for the health system and models of health care delivery. For example, a recent study in a peri-urban informal township near Cape Town, South Africa showed that 19% of HIV-infected patients on ART were on treatment for another chronic disease, with 77% and 17% of these patients concurrently receiving anti-hypertensive and diabetic treatment respectively. 98 There is therefore a need to ensure integrated care across the continuum of care from primary to tertiary levels.
The Innovative Care for Chronic Conditions (ICCC) Framework developed by WHO addresses the increasing burden of chronic diseases in LMIC and is a tool designed to assist health systems to shift from providing predominantly acute episodic care in order to meet the increasing needs of chronic disease care. 99 However, it does not explicitly incorporate the concept of co-existing and interacting multiple morbidities in these settings. A conceptual modification to this framework has been proposed that incorporates these multiple morbidities and examines the impact beyond biological interaction of these diseases. 100 This modified framework could be used as a tool to help guide the development of integrated interventions at multiple levels. Models for integration of commonly occurring conditions need to be evaluated to optimize and streamline management. Integrated chronic disease models are being developed and implemented in some LMIC. An example is the integrated chronic disease management model in South Africa that includes HIV, TB, diabetes, hypertension, asthma, epilepsy, asthma, COPD and mental health illnesses. This model builds on the strengths of the HIV/TB integrated programme and focuses on a systems approach to re-structuring the primary health care system, improving efficiency using integrated clinical algorithms, clinic stationery and re-organised clinic flows as well as the integrated training of community care workers in the prevention, promotion and treatment of these diseases. In the context of multimorbidity, the model also aims to empower patients and assist with self-management of their chronic diseases. Integration of community support groups is another approach to supporting patients with multiple and interacting chronic diseases potentially improving adherence to treatment and disease outcomes.
When considering interventions aimed at primary prevention, Figure 2 highlights the importance, both of considering shared risk factors (identified in Figure 1 ) that influence the risk and outcomes, and of using a life course approach when considering targets for intervention. Women have a disproportionally higher prevalence of certain NCD risk factors, particularly obesity and lower physical activity, and in addition show rising rates of smoking and alcohol consumption. 101 Given this fact, along with the impact of maternal factors on fetal and child health, and the likelihood of strongly influencing dietary household choices, female adolescents and adults represent an important population group for intervention. These interventions should ideally occur pre-conception and cover nutrition, physical activity, contraception, high-risk behavior including high-risk sexual practices, smoking and alcohol consumption. Figure 2 also highlights the importance of focusing on the elderly as ageing is associated with increasing prevalence of NCDs and an increased susceptibility to communicable diseases. With increasing access to ART, there is increasing survival and ageing in HIV-infected persons. However, public health HIV control interventions in LMIC often focus on the younger 15–44 age group where incidence is highest, with insufficient emphasis on the older age groups. Furthermore, immunocompromise associated with ageing increases the risk of other communicable diseases including TB, potentially compounded by the increased risk of T2DM. Given the high prevalence of NCDs, older persons in LMIC are at a high risk of developing multi-morbid communicable and non-communicable conditions. 102 This can result in disability, reduced quality of life, and social isolation, limiting their ability to fulfill emotional, cultural and economic roles within families and the society. Interventions that address isolation and promote social participation have been identified as potentially important in the elderly. 103
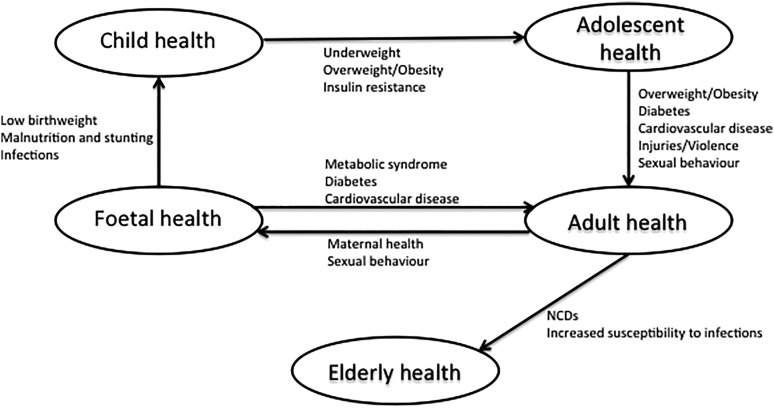
Life-course approach to joint communicable and non-communicable disease (NCD) prevention and control.
Limitations
As this is a critical and not a systematic review it did not aim to exhaustively identify and abstract data from all relevant literature. Rather the aim was to describe key concepts from the current literature. While we believe that we have achieved this aim, it is quite possible that other authors would have used somewhat different literature to illustrate the same concepts.
Conclusions
The aim of this review was to illustrate the overlap and interaction between communicable and NCDs, particularly in LMIC, and show how the agendas for their prevention and control are inextricably linked. There is therefore a need for those responsible for the design of health systems within individual countries to understand the distribution and interaction of communicable and NCDs within their own populations in order to appropriately plan preventive and treatment programs and services. When it comes to the provision of health care for treatment this will require breaking down barriers between departments within health ministries that have traditionally designed services and programs for communicable and NCDs separately. When it comes to prevention, it will require integrated multi-sectoral action addressing determinants across the life course.
Acknowledgments
Authors' contributions : TO and NU were responsible for conceptualizing the manuscript. TO led the writing, with both TO and NU contributing to initial drafts of the manuscript and editing. TO and NU read and approved the final manuscript. TO is guarantor of the paper.
Funding : This work was supported by a Carnegie Corporation Postdoctoral Fellowship; a Harry Crossley Senior Clinical Fellowship; a Wellcome Trust funded Clinical Infectious Disease Research Initiative clinical fellow postdoctoral award; and the University of the West Indies.
Competing interests : None declared.
Ethical approval : Not required.
- 1. World Bank Group. Data. Country and Lending Groups. http://data.worldbank.org/about/country-and-lending-groups [accessed 29 March 2015.
- 2. Setel PW, Saker L, Unwin N et al. . Is it time to reassess the categorization of disease burdens in low-income countries? Am J Public Health 2004;94:384. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 3. Omran AR. The epidemiologic transition: a theory of the epidemiology of population change. Milbank Q 2005;83:731–57. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 4. Nelson MC, Rogers J. The epidemiologic transition revisited, or what happenes if we look beneath the surface? Health Transit Rev 1997;7:235–55. [ Google Scholar ]
- 5. Santosa A, Wall S, Fottrell E et al. . The development and experience of epidemiological transition theory over four decades: a systematic review. Glob Health Action 2014;7:23574. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 6. Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J 2009;26:91–108. [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. WHO. Global Tuberculosis Report 2014. Geneva: World Health Organization; 2014. [ Google Scholar ]
- 8. Lönnroth K, Roglic G, Harries AD. Improving tuberculosis prevention and care through addressing the global diabetes epidemic: from evidence to policy and practice. Lancet Diabetes Endocrinol 2014;2:730–9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. WHO. Global Strategy and Targets for Tuberculosis Prevention, Care, and Control After 2015. WHO 67th World Health Assembly 2014 Geneva: World Health Organization; 2014. [ Google Scholar ]
- 10. Patra J, Jha P, Rehm J, Suraweera W. Tobacco smoking, alcohol drinking, diabetes, low body mass index and the risk of self-reported symptoms of active tuberculosis: individual participant data (IPD) meta-analyses of 72,684 individuals in 14 high tuberculosis burden countries. PLoS ONE 2014;9:e96433. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 11. Jeon CY, Murray MB. Diabetes mellitus increases the risk of active tuberculosis: a systematic review of 13 observational studies. PLoS Med 2008;5:e152. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 12. Stevenson CR, Critchley JA, Forouhi NG et al. . Diabetes and the risk of tuberculosis: a neglected threat to public health? Chronic Illn 2007;3:228–45. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Riza AL, Pearson F, Ugarte-Gil C et al. . Clinical management of concurrent diabetes and tuberculosis and the implications for patient services. Lancet Diabetes Endocrinol 2014;2:740–53. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 14. Faurholt-Jepsen D, Range N, Praygod G et al. . Diabetes is a risk factor for pulmonary tuberculosis: a case-control study from Mwanza, Tanzania. PLoS ONE 2011;6:e24215. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 15. Baker MA, Harries AD, Jeon CY et al. . The impact of diabetes on tuberculosis treatment outcomes: a systematic review. BMC Med 2011;9:81. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 16. International Diabetes Federation. Diabetes Atlas. Give edition. http://www.idf.org/diabetesatlas [accessed 17 November 2013].
- 17. Van Crevel R, Dockrell HM. TANDEM: understanding diabetes and tuberculosis. Lancet Diabetes Endocrinol 2014;2:270–2. [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Lee C-H, Lee M-C, Shu C-C et al. . Risk factors for pulmonary tuberculosis in patients with chronic obstructive airway disease in Taiwan: a nationwide cohort study. BMC Infect Dis 2013;13:194. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. Inghammar M, Ekbom A, Engström G et al. . COPD and the risk of tuberculosis--a population-based cohort study. PLoS ONE 2010;5:e10138. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 20. Lin H-H, Ezzati M, Murray M. Tobacco smoke, indoor air pollution and tuberculosis: a systematic review and meta-analysis. PLoS Med 2007;4:e20. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 21. Allwood BW, Myer L, Bateman ED. A systematic review of the association between pulmonary tuberculosis and the development of chronic airflow obstruction in adults. Respiration 2013;86:76–85. [ DOI ] [ PubMed ] [ Google Scholar ]
- 22. Pasipanodya JG, Miller TL, Vecino M et al. . Pulmonary impairment after tuberculosis. Chest 2007;131:1817–24. [ DOI ] [ PubMed ] [ Google Scholar ]
- 23. Willcox PA, Ferguson AD. Chronic obstructive airways disease following treated pulmonary tuberculosis. Respir Med 1989;83:195–8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 24. Hnizdo E, Singh T, Churchyard G. Chronic pulmonary function impairment caused by initial and recurrent pulmonary tuberculosis following treatment. Thorax 2000;55:32–8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 25. Jordan TS, Spencer EM, Davies P. Tuberculosis, bronchiectasis and chronic airflow obstruction. Respirology 2010;15:623–8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 26. Maguire GP, Anstey NM, Ardian M et al. . Pulmonary tuberculosis, impaired lung function, disability and quality of life in a high-burden setting. Int J Tuberc Lung Dis 2009;13:1500–6. [ PubMed ] [ Google Scholar ]
- 27. Ehrlich RI, White N, Norman R et al. . Predictors of chronic bronchitis in South African adults. Int J Tuberc Lung Dis 2004;8:369–76. [ PubMed ] [ Google Scholar ]
- 28. Barsoum RS. Chronic kidney disease in the developing world. N Engl J Med 2006;354:10. [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. Hussein M, Mooij J. Tuberculosis and chronic renal disease. Saudi J Kidney Dis Transpl 2002;320–30. [ PubMed ] [ Google Scholar ]
- 30. Venkata RK, Kumar S, Krishna RP et al. . Tuberculosis in chronic kidney disease. Clin Nephrol 2007;67:217–20. [ DOI ] [ PubMed ] [ Google Scholar ]
- 31. Ates G, Yildiz T, Danis R et al. . Incidence of tuberculosis disease and latent tuberculosis infection in patients with end stage renal disease in an endemic region. Ren Fail 2010;32:91–5. [ DOI ] [ PubMed ] [ Google Scholar ]
- 32. Reis-Santos B, Gomes T, Horta BL, Maciel EL. The outcome of tuberculosis treatment in subjects with chronic kidney disease in Brazil: a multinomial analysis. J Bras Pneumol 39:585. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 33. Sharma AP, Sural S, Gupta A et al. . Effect of antitubercular medications on blood pressure control in chronic kidney disease patients with tuberculosis: a prospective cohort study. J Nephrol 2006;19:771–7. [ PubMed ] [ Google Scholar ]
- 34. Desai HN. Tuberculous pericarditis. A review of 100 cases. S Afr Med J 1979;55:877–80. [ PubMed ] [ Google Scholar ]
- 35. Mayosi BM, Burgess LJ, Doubell AF. Tuberculous pericarditis. Circulation 2005;112:3608–16. [ DOI ] [ PubMed ] [ Google Scholar ]
- 36. Reuter H, Burgess LJ, Doubell AF. Epidemiology of pericardial effusions at a large academic hospital in South Africa. Epidemiol Infect 2005;133:393–9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 37. Murray CJL, Vos T, Lozano R et al. . Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2197–223. [ DOI ] [ PubMed ] [ Google Scholar ]
- 38. Lozano R, Naghavi M, Foreman K et al. . Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2095–128. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 39. WHO, UNAID, UNICEF. Global HIV/AIDS Response: Epidemic update and health sector progress towards Universal Access – Progress Report 2011. Geneva: World Health Organization; 2011. http://www.unaids.org/sites/default/files/media_asset/20111130_UA_Report_en_1.pdf [accessed 1 December 2014]. [ Google Scholar ]
- 40. Subbaraman R, Chaguturu SK, Mayer KH et al. . Adverse effects of highly active antiretroviral therapy in developing countries. Clin Infect Dis 2007;45:1093–1101. [ DOI ] [ PubMed ] [ Google Scholar ]
- 41. Dillon DG, Gurdasani D, Riha J et al. . Association of HIV and ART with cardiometabolic traits in sub-Saharan Africa: a systematic review and meta-analysis. Int J Epidemiol 2013;42:1754–71. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 42. Walker RW, Jusabani A, Aris E et al. . Stroke risk factors in an incident population in urban and rural Tanzania: a prospective, community-based, case-control study. Lancet Glob Health 1:e282–8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 43. Butt AA, McGinnis K, Rodriguez-Barradas MC et al. . HIV infection and the risk of diabetes mellitus. AIDS 2009;23:1227–34. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 44. Brown TT, Cole SR, Li X et al. . Antiretroviral therapy and the prevalence and incidence of diabetes mellitus in the multicenter AIDS cohort study. Arch Intern Med 2005;165:1179–84. [ DOI ] [ PubMed ] [ Google Scholar ]
- 45. De Wit S, Sabin CA, Weber R et al. . Incidence and risk factors for new-onset diabetes in HIV-infected patients: the Data Collection on Adverse Events of Anti-HIV Drugs (D:A:D) study. Diabetes Care 2008;31:1224–9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 46. Samaras K. Prevalence and pathogenesis of diabetes mellitus in HIV-1 infection treated with combined antiretroviral therapy. J Acquir Immune Defic Syndr 2009;50:499–505. [ DOI ] [ PubMed ] [ Google Scholar ]
- 47. Dave JA, Lambert EV, Badri M et al. . Effect of nonnucleoside reverse transcriptase inhibitor-based antiretroviral therapy on dysglycemia and insulin sensitivity in South African HIV-infected patients. J Acquir Immune Defic Syndr 2011;57:284–9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 48. Grunfeld C, Kotler DP, Hamadeh R et al. . Hypertriglyceridemia in the acquired immunodeficiency syndrome. Am J Med. 1989;86:27–31. [ DOI ] [ PubMed ] [ Google Scholar ]
- 49. Montes ML, Pulido F, Barros C et al. . Lipid disorders in antiretroviral-naive patients treated with lopinavir/ritonavir-based HAART: frequency, characterization and risk factors. J Antimicrob Chemother 2005;55:800–4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 50. Anastos K, Lu D, Shi Q et al. . Association of serum lipid levels with HIV serostatus, specific antiretroviral agents, and treatment regimens. J Acquir Immune Defic Syndr 2007;45:34–42. [ DOI ] [ PubMed ] [ Google Scholar ]
- 51. Goedecke JH, Micklesfield LK, Levitt NS et al. . Effect of different antiretroviral drug regimens on body fat distribution of HIV-infected South African women. AIDS Res Hum Retroviruses 2013;29:557–63. [ DOI ] [ PubMed ] [ Google Scholar ]
- 52. Thienemann F, Sliwa K, Rockstroh JK. HIV and the heart: the impact of antiretroviral therapy: a global perspective. Eur Heart J 2013; 34:3538–46. [ DOI ] [ PubMed ] [ Google Scholar ]
- 53. Twagirumukiza M, Nkeramihigo E, Seminega B et al. . Prevalence of dilated cardiomyopathy in HIV-infected African patients not receiving HAART: a multicenter, observational, prospective, cohort study in Rwanda. Curr HIV Res 2007;5:129–37. [ DOI ] [ PubMed ] [ Google Scholar ]
- 54. Luo L, Ye Y, Liu Z et al. . Assessment of cardiac diastolic dysfunction in HIV-infected people without cardiovascular symptoms in China. Int J STD AIDS 2010;21:814–8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 55. Sliwa K, Carrington MJ, Becker A et al. . Contribution of the human immunodeficiency virus/acquired immunodeficiency syndrome epidemic to de novo presentations of heart disease in the Heart of Soweto Study cohort. Eur Heart J 2012;33:866–74. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 56. Chillo P, Bakari M, Lwakatare J. Echocardiographic diagnoses in HIV-infected patients presenting with cardiac symptoms at Muhimbili National Hospital in Dar es Salaam, Tanzania. Cardiovasc J Africa 2012;23:90–7. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 57. Thöni GJ, Schuster I, Walther G et al. . Silent cardiac dysfunction and exercise intolerance in HIV+ men receiving combined antiretroviral therapies. AIDS 2008;22:2537–40. [ DOI ] [ PubMed ] [ Google Scholar ]
- 58. Reinsch N, Kahlert P, Esser S et al. . Echocardiographic findings and abnormalities in HIV-infected patients: results from a large, prospective, multicenter HIV-heart study. Am J Cardiovasc Dis 2011;1:176–84. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 59. Degano B, Guillaume M, Savale L et al. . HIV-associated pulmonary arterial hypertension: survival and prognostic factors in the modern therapeutic era. AIDS 2010;24:67–75. [ DOI ] [ PubMed ] [ Google Scholar ]
- 60. Young F, Critchley JA, Johnstone LK, Unwin NC. A review of co-morbidity between infectious and chronic disease in Sub Saharan Africa: TB and diabetes mellitus, HIV and metabolic syndrome, and the impact of globalization. Global Health 2009;5:9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 61. D:A:D Study Group Sabin CA, Worm SW et al. . Use of nucleoside reverse transcriptase inhibitors and risk of myocardial infarction in HIV-infected patients enrolled in the D:A:D study: a multi-cohort collaboration. Lancet 2008;371:1417–26. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 62. Lang S, Mary-Krause M, Cotte L et al. . Impact of individual antiretroviral drugs on the risk of myocardial infarction in human immunodeficiency virus-infected patients: a case-control study nested within the French Hospital Database on HIV ANRS cohort CO4. Arch Intern Med 2010;170:1228–38. [ DOI ] [ PubMed ] [ Google Scholar ]
- 63. Monforte AD, Reiss P, Ryom L et al. . Atazanavir is not associated with an increased risk of cardio- or cerebrovascular disease events. AIDS 2013;27:407–15. [ DOI ] [ PubMed ] [ Google Scholar ]
- 64. Ding X, Andraca-Carrera E, Cooper C et al. . No association of abacavir use with myocardial infarction: findings of an FDA meta-analysis. J Acquir Immune Defic Syndr 2012;61:441–7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 65. Szczech LA, Gupta SK, Habash R et al. . The clinical epidemiology and course of the spectrum of renal diseases associated with HIV infection. Kidney Int 2004;66:1145–52. [ DOI ] [ PubMed ] [ Google Scholar ]
- 66. Winston J, Deray G, Hawkins T et al. . Kidney disease in patients with HIV infection and AIDS. Clin Infect Dis 2008;47:1449–57. [ DOI ] [ PubMed ] [ Google Scholar ]
- 67. Berns JS, Kasbekar N. Highly active antiretroviral therapy and the kidney: an update on antiretroviral medications for nephrologists. Clin J Am Soc Nephrol 2006;1:117–29. [ DOI ] [ PubMed ] [ Google Scholar ]
- 68. Hsieh M-H, Lu P-L, Kuo M-C et al. . Prevalence of and associated factors with chronic kidney disease in human immunodeficiency virus-infected patients in Taiwan. J Microbiol Immunol Infect 2013; pii:S1684–1182(13)00158–8.check page numbers [ DOI ] [ PubMed ] [ Google Scholar ]
- 69. Mizushima D, Tanuma J, Kanaya F et al. . WHO antiretroviral therapy guidelines 2010 and impact of tenofovir on chronic kidney disease in Vietnamese HIV-infected patients. PLoS One 2013;8:e79885. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 70. Kalyesubula R, Perazella MA. Nephrotoxicity of HAART. AIDS Res Treat 2011;2011:1–11. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 71. Diaz PT, King MA, Pacht ER et al. . Increased susceptibility to pulmonary emphysema among HIV-seropositive smokers. Ann Intern Med 2000;132:369–72. [ DOI ] [ PubMed ] [ Google Scholar ]
- 72. O'Donnell CR, Bader MB, Zibrak JD et al. . Abnormal airway function in individuals with the acquired immunodeficiency syndrome. Chest 1988;94:945–8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 73. Crothers K, Butt AA, Gibert CL et al. . Increased COPD among HIV-positive compared to HIV-negative veterans. Chest 2006;130:1326–33. [ DOI ] [ PubMed ] [ Google Scholar ]
- 74. Gingo MR, Balasubramani GK, Rice TB et al. . Pulmonary symptoms and diagnoses are associated with HIV in the MACS and WIHS cohorts. BMC Pulm Med 2014;14:75. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 75. Madeddu G, Fois AG, Calia GM et al. . Chronic obstructive pulmonary disease: an emerging comorbidity in HIV-infected patients in the HAART era? Infection 2012;41:347–53. [ DOI ] [ PubMed ] [ Google Scholar ]
- 76. Makinson A, Hayot M, Eymard-Duvernay S et al. . High prevalence of undiagnosed COPD in a cohort of HIV-infected smokers. Eur Resp J 2014;pii: erj01549–2014. [ DOI ] [ PubMed ] [ Google Scholar ]
- 77. High KP, Brennan-Ing M, Clifford DB et al. . HIV and aging. J Acquir Immune Defic Syndr 2012;60:S1–18. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 78. Yusuf AJ, Hassan A, Mamman AI et al. . Prevalence of HIV-associated neurocognitive disorder (HAND) among patients attending a tertiary health facility in Northern Nigeria. J Int Assoc Provid AIDS Care 2014; pii: 23259557414553839. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 79. Garg RK. HIV infection and seizures. Postgrad Med J 1999;75:387. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 80. Satishchandra P, Sinha S. Seizures in HIV-seropositive individuals: NIMHANS experience and review. Epilepsia 2008;49:33–41. [ DOI ] [ PubMed ] [ Google Scholar ]
- 81. Epilepsy and HIV-a dangerous combination. Lancet Neurol 2007;6:747. [ DOI ] [ PubMed ] [ Google Scholar ]
- 82. Birbeck GL, French JA, Perucca E et al. . Evidence-based guideline: Antiepileptic drug selection for people with HIV/AIDS: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Ad Hoc Task Force of the Commission on Therapeutic Strategies of the International League Against Epilepsy. Neurology 2012;78:139–45. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 83. Siddiqi O, Birbeck GL. Safe Treatment of seizures in the setting of HIV/AIDS. Curr Treat Options Neurol 2013;15:529–43. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 84. WHO. Malaria: fact sheet no. 94. Geneva: World Health Organization; 2013. [ Google Scholar ]
- 85. Gething PW, Patil AP, Smith DL et al. . A new world malaria map: Plasmodium falciparum endemicity in 2010. Malar J 2011;10:378. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 86. Tusting LS, Willey B, Lucas H et al. . Socioeconomic development as an intervention against malaria: a systematic review and meta-analysis. Lancet 2013;382:963–72. [ DOI ] [ PubMed ] [ Google Scholar ]
- 87. Perez-Escamilla R, Dessalines M, Finnigan M et al. . Household food insecurity is associated with childhood malaria in rural Haiti. J Nutr 2009;139:2132–8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 88. Mitangala PN, D'Alessandro U, Donnen P et al. . Malaria infection and nutritional status: results from a cohort survey of children from 6–59 months old in the Kivu province, Democratic Republic of the Congo. Rev Epidemiol Sante Publique 2013;61:111–20. [ DOI ] [ PubMed ] [ Google Scholar ]
- 89. Deribew A, Alemseged F, Tessema F et al. . Malaria and under-nutrition: a community based study among under-five children at risk of malaria, south-west Ethiopia. PLoS One 2010;5:e10775. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 90. Crookston BT, Alder SC, Boakye I et al. . Exploring the relationship between chronic undernutrition and asymptomatic malaria in Ghanaian children. Malar J 2010;9:39. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 91. Danquah I, Bedu-Addo G, Mockenhaupt FP. Type 2 diabetes mellitus and increased risk for malaria infection. Emerg Infect Dis 2010;16:1601–4. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 92. Jha V, Garcia-Garcia G, Iseki K et al. . Chronic kidney disease: global dimension and perspectives. Lancet 2013;382:260–72. [ DOI ] [ PubMed ] [ Google Scholar ]
- 93. White SL, Chadban SJ, Jan S et al. . How can we achieve global equity in provision of renal replacement therapy? Bull World Health Organ 2008;86:229–37. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 94. Anand S, Bitton A, Gaziano T. The gap between estimated incidence of end-stage renal disease and use of therapy. PLoS One 2013;8:e72860. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 95. Elsheikha HM, Sheashaa HA. Epidemiology, pathophysiology, management and outcome of renal dysfunction associated with plasmodia infection. Parasitol Res 2007;101:1183–90. [ DOI ] [ PubMed ] [ Google Scholar ]
- 96. NICE. Malaria prophylaxis. London: National Institute for Health and Care Excellence; 2012. http://cks.nice.org.uk/malaria-prophylaxis [accessed 15 December 2014]. [ Google Scholar ]
- 97. Collins WE, Jeffery GM. Plasmodium malariae : parasite and disease. Clin Microbiol Rev 2007;20:579–92. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 98. Oni T, Youngblood E, Boulle A et al. . Patterns of HIV, TB, and non-communicable disease multi-morbidity in peri-urban South Africa- a cross sectional study. BMC Infect Dis 2015;15:20. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 99. WHO. Diabetes Programme. Innovative care for chronic conditions: Building blocks for action: WHO global report 2002. Geneva: World Health Organization; 2002. http://www.who.int/diabetes/publications/icccreport/en/ [accessed 1 December 2014]. [ Google Scholar ]
- 100. Oni T, McGrath N, BeLue R et al. . Chronic diseases and multi-morbidity - a conceptual modification to the WHO ICCC model for countries in health transition. BMC Public Health 2014;14:575. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 101. WHO. Global Status Report on Non-Communicable Diseases 2010. Geneva: World Health Organization; 2011. http://www.who.int/nmh/publications/ncd_report_full_en.pdf [accessed 20 January 2015]. [ Google Scholar ]
- 102. WHO. Global Health and Aging. Geneva: World Health Organization; 2011. http://www.who.int/ageing/publications/global_health.pdf [accessed 20 January 2015]. [ Google Scholar ]
- 103. Holmes WR, Joseph J. Social participation and healthy ageing: a neglected, significant protective factor for chronic non communicable conditions. Global Health 2011;7:43. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (389.2 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

IMAGES
VIDEO
COMMENTS
Human disease - Classifications, Causes, Symptoms: Classifications of diseases become extremely important in the compilation of statistics on causes of illness (morbidity) and causes of death (mortality). It is obviously important to know what kinds of illness and disease are prevalent in an area and how these prevalence rates vary with time. Classifying diseases made it apparent, for example ...
This type refers to the affected organ or tissue. Heart disease. Topographical Classification. Further classified into types such as vascular disease, chest disease, gastrointestinal disease, and abdominal diseases. These are then handled by specializations in medicine that follow these topographical classifications.
Students are often asked to write an essay on Diseases in their schools and colleges. And if you're also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic. ... Classification of Diseases. Diseases are classified into two main categories: infectious and non-infectious. Infectious diseases are caused by ...
classification of diseases validates, locates, and distributes: ... This essay will use the w ork of these individuals as a starting point. Perspectives in Biology and Medicine.
Originally designed as a classification scheme for health care, the ICD provides a scheme of diagnostic codes for classification of illnesses, including nuanced classifications of a broad range of signs, symptoms, unusual results, complaints, social conditions and external causes of injury or disease.
The aim of this essay is to synthesize key analytical perspectives on disease classification across these scholarly fields in order to guide analyses of current developments in precision medicine. 2 I argue that attention to the past is needed to grasp contemporary changes in disease classifications because new diagnostic techniques and ...
Classical classification of human disease derives from the observational correlation between pathological analysis and clinical syndromes. Today it is preferred to classify them by their cause if it is known. [24] The most known and used classification of diseases is the World Health Organization's ICD. This is periodically updated.
Cell cycle The process by which a cell divides into two cells. The cycle usually follows the four stages: G 1 (gap or growth 1), S (synthesis of DNA), G 2 (gap or growth 2), finally mitosis (note in meiosis, the cell cycle follows a different pattern, as described below). G 1, S and G 2 together make up 'interphase'.
The International Classification of Diseases (ICD) has long been the main basis for comparability of statistics on causes of mortality and morbidity between places and over time. This paper provides an overview of the recently completed 11th revision of the ICD, focusing on the main innovations and their implications. Changes in content reflect knowledge and perspectives on diseases and their ...
For more than a century, the International Classification of Diseases (ICD) has been the basis for comparable statistics on causes of mortality and morbidity between places and over time. Originating in the 19 th century, the latest version of the ICD, ICD-11, was adopted by the 72 nd World Health Assembly in 2019 and came into effect on 1 st ...
disease, any harmful deviation from the normal structural or functional state of an organism, generally associated with certain signs and symptoms and differing in nature from physical injury.A diseased organism commonly exhibits signs or symptoms indicative of its abnormal state. Thus, the normal condition of an organism must be understood in order to recognize the hallmarks of disease.
Disclaimer: This essay is provided as an example of work produced by students studying towards a biology degree, ... A classification system for diseases database is very usefulfor reporting and monitoring diseases.This allows the world to compare and share data in a consistent and standard way - between professionals and hospitals. ...
Some of the bacterial diseases are Syphilis, Pneumonia, Tetanus, and Tuberculosis. Examples of diseases caused by a virus are Chickenpox, Small Pox, Measles, Polio. Fungal infections include Ringworm infection, Athlete's foot, Yeast infections etc. Malaria is a disease caused by an organism belonging to Protista.
public health - Student Encyclopedia (Ages 11 and up) International Classification of Diseases (ICD), in medicine, diagnostic tool that is used to classify and monitor causes of injury and death and that maintains information for health analyses, such as the study of mortality (death) and morbidity (illness) trends. The ICD is designed to promote.
The book is divided into three sections: classification, disease and evidence. In general, attention is focused on statistics in medicine and epidemiology, issues in psychiatry and connecting medicine with evolutionary biology and genetics. Many authors position the theories that they address within their historical contexts.
WHO classification of disease. There are many different ways to classify diseases, but one of the most commonly used systems is the International Classification of Diseases (ICD). The ICD is published by the World Health Organization and provides a standard way of classifying both physical and mental disorders. The ICD is regularly updated to ...
Noncommunicable diseases (NCDs), also known as chronic diseases, are not passed from person to person. They are of long duration and generally slow progression. The four main types of noncommunicable diseases are cardiovascular diseases (like heart attacks and stroke), cancers, chronic respiratory diseases (such as chronic obstructive pulmonary disease and asthma) and diabetes.
As the editors of Classification, Disease and Evidence note, "philosophical topics have direct ethical consequences" (xv). The book comprises ten essays that present a sampling of recent work in the philosophy of medicine. It is nominally organized around the three concepts in the title, but in the order Disease, Classification, and Evidence.
Ask the Chatbot a Question Ask the Chatbot a Question infectious disease, in medicine, a process caused by an agent, often a type of microorganism, that impairs a person's health.In many cases, infectious disease can be spread from person to person, either directly (e.g., via skin contact) or indirectly (e.g., via contaminated food or water). An infectious disease can differ from simple ...
The broad classification of diseases into communicable (infectious) and non-communicable diseases (NCDs) is deeply ingrained. ... Both authors identified and reviewed papers and 80 articles were eventually included in the review. Of note, there was a lot of information about the NCDs and TB or HIV interactions but far fewer studies on malaria ...
Gastrointestinal (GI) diseases are a significant global health issue, causing millions of deaths annually. This study presents a novel method for classifying GI diseases using endoscopy videos. The proposed method involves three major phases: image processing, feature extraction, and classification.