Advertisement

Cervical cancer in Ethiopia: a review of the literature
- Review article
- Published: 15 October 2022
- Volume 34 , pages 1–11, ( 2023 )
Cite this article

- Awoke Derbie ORCID: orcid.org/0000-0002-6949-3494 1 , 2 , 3 , 4 ,
- Daniel Mekonnen 1 , 3 ,
- Endalkachew Nibret 5 ,
- Eyaya Misgan 6 ,
- Melanie Maier 7 ,
- Yimtubezinash Woldeamanuel 2 , 4 &
- Tamrat Abebe 4
2286 Accesses
11 Citations
1 Altmetric
Explore all metrics
Cervical cancer is one of the most common malignancies affecting women worldwide with large geographic variations in prevalence and mortality rates. It is one of the leading causes of cancer-related deaths in Ethiopia, where vaccination and screening are less implemented. However, there is a scarcity of literature in the field. Therefore, the objective of this review was to describe current developments in cervical cancer in the Ethiopian context. The main topics presented were the burden of cervical cancer, knowledge of women about the disease, the genotype distribution of Human papillomavirus (HPV), vaccination, and screening practices in Ethiopia.
Published literature in the English language on the above topics until May 2021 were retrieved from PubMed/Medline, SCOPUS, Google Scholar, and the Google database using relevant searching terms. Combinations of the following terms were considered to retrieve literature; < Cervical cancer, uterine cervical neoplasms, papillomavirus infections, papillomavirus vaccines, knowledge about cervical cancer, genotype distribution of HPV and Ethiopia > . The main findings were described thematically.
Cervical cancer is the second most common and the second most deadly cancer in Ethiopia, The incidence and prevalence of the disease is increasing from time to time because of the growth and aging of the population, as well as an increasing prevalence of well-established risk factors. Knowledge and awareness about cervical cancer is quite poor among Ethiopian women. According to a recent report (2021), the prevalence of previous screening practices among Ethiopian women was at 14%. Although HPV 16 is constantly reported as the common genotype identified from different grade cervical lesions in Ethiopia, studies reported different HPV genotype distributions across the country. According to a recent finding, the most common HPV types identified from cervical lesions in the country were HPV-16, HPV-52, HPV-35, HPV-18, and HPV-56. Ethiopia started vaccinating school girls using Gardasil-4™ in 2018 although the coverage is insignificant. Recently emerging reports are in favor of gender-neutral vaccination strategies with moderate coverage that was found superior and would rapidly eradicate high-risk HPVs than vaccinating only girls.
Conclusions
Cervical cancer continues to be a major public health problem affecting thousands of women in Ethiopia. As the disease is purely preventable, classic cervical cancer prevention strategies that include HPV vaccination using a broad genotype coverage, screening using a high precision test, and treating cervical precancerous lesions in the earliest possible time could prevent most cervical cancer cases in Ethiopia. The provision of a focused health education supported by educational materials would increase the knowledge of women about cervical cancer in general and the uptake of cervical cancer prevention and screening services in particular.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Price excludes VAT (USA) Tax calculation will be finalised during checkout.
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Adopted from WHO ( Guidelines for screening and treatment of precancerous lesions for cervical cancer prevention, 2013) . Program managers and decision-makers can start at the top and answer the questions accordingly to determine which screen-and-treat option is best in the context where it will be implemented. It highlights choices related to resources, which can include costs, staff and training
Similar content being viewed by others
Human papillomavirus genotype distribution in Ethiopia: an updated systematic review

National genotype prevalence and age distribution of human papillomavirus from infection to cervical cancer in Japanese women: a systematic review and meta-analysis protocol

Factors Influencing the Cost-Effectiveness Outcomes of HPV Vaccination and Screening Interventions in Low-to-Middle-Income Countries (LMICs): A Systematic Review
Data availability.
All the generated data are included in the manuscript.
Abbreviations
Cervical intraepithelial neoplasia
Human papillomavirus
International agency for research on cancer
Sexually transmitted disease
Visual inspection of the cervix with acetic acid
World health organization
Hull R, Mbele M, Makhafola T, Hicks C, Wang S-M, Reis RM, Mehrotra R, Mkhize-Kwitshana Z, Kibiki G, Bates DO et al (2020) Cervical cancer in low and middle-income countries. Oncol Lett 20(3):2058–2074
Article CAS Google Scholar
World Health Organization (WHO). Cervical cancer. Available from ( http://www.who.int/news-room/fact-sheets/detail/cervical-cancer) . Accessed on 17 Aug 2022
Cancer tomorrow: estimated number of cervical cancer incidence and mortality in Ethiopia ( https://gco.iarc.fr/tomorrow/en/dataviz/isotype?cancers=23&single_unit=500&populations=231&group_populations=1&multiple_populations=1&sexes=0&types=1&age_start=0 )
Integrated Africa cancer factsheet focusing on cervical cancer ( http://www.who.int/pmnch/media/events/2014/africa_cancer_factsheet.pdf )
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer J Clin 68(6):394–424
Google Scholar
De Vuyst H, Alemany L, Lacey C, Chibwesha CJ, Sahasrabuddhe V, Banura C, Denny L, Parham GP (2013) The burden of human papillomavirus infections and related diseases in sub-saharan Africa. Vaccine 31(5):F32-46
Article Google Scholar
Cohen PA, Jhingran A, Oaknin A, Denny L (2019) Cervical cancer. Lancet 393(10167):169–182
Forman D, de Martel C, Lacey CJ, Soerjomataram I, Lortet-Tieulent J, Bruni L, Vignat J, Ferlay J, Bray F, Plummer M et al (2012) Global burden of human papillomavirus and related diseases. Vaccine 30(Suppl 5):F12-23
WHO: Guidelines for screening and treatment of precancerous lesions for cervical cancer prevention. In: World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland 2013.
HPV detection and genotyping using the luminex xMAP technology ( http://www.irma-international.org/viewtitle/40440/ )
Maine D, Hurlburt S, Greeson D (2011) Cervical cancer prevention in the 21st century: cost is not the only issue. Am J Public Health 101(9):1549–1555
Santos-Lopez G, Marquez-Dominguez L, Reyes-Leyva J, Vallejo-Ruiz V (2015) General aspects of structure, classification and replication of human papillomavirus. Rev Med Inst Mex Seguro Soc 53(2):S166-171
Human papillomavirus (HPV) and cervical cancer ( http://www.who.int/mediacentre/factsheets/fs380/en/ )
ICO/IARC information centre on HPV and cancer (HPV information centre). Human papillomavirus and related diseases in the world. Summary report 2017. ( http://www.hpvcentre.net/statistics/reports/XWX.pdf )
Chow LT, Broker TR, Steinberg BM (2010) The natural history of human papillomavirus infections of the mucosal epithelia. APMIS 118(6–7):422–449
Doorbar J, Quint W, Banks L, Bravo IG, Stoler M, Broker TR, Stanley MA (2012) The biology and life-cycle of human papillomaviruses. Vaccine 20(30):083
Wallace NA, Galloway DA (2015) Novel functions of the human papillomavirus E6 oncoproteins. Annu Rev Virol 2(1):403–423
Human papillomavirus and related diseases report ( http://www.hpvcentre.net/statistics/reports/XWX.pdf )
Yugawa T, Kiyono T (2009) Molecular mechanisms of cervical carcinogenesis by high-risk human papillomaviruses: novel functions of E6 and E7 oncoproteins. Rev Med Virol 19(2):97–113
Yugawa T, Kiyono T (2008) Molecular basis of cervical carcinogenesis by high-risk human papillomaviruses. Uirusu 58(2):141–154
Arbyn M, Weiderpass E, Bruni L, de Sanjosé S, Saraiya M, Ferlay J, Bray F (2020) Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health 8(2):e191–e203
Anorlu RI (2008) Cervical cancer: the sub-Saharan African perspective. Reprod Health Matters 16(32):41–49
Cervical Cancer ( https://www.afro.who.int/health-topics/cervical-cancer )
Jedy-Agba E, Joko WY, Liu B, Buziba NG, Borok M, Korir A, Masamba L, Manraj SS, Finesse A, Wabinga H et al (2020) Trends in cervical cancer incidence in sub-Saharan Africa. Br J Cancer 123(1):148–154
25ICO/IARCInformation Centre on HPV and Cancer (HPV Information Centre). Human papillomavirus and related diseases in Ethiopia. ( https://hpvcentre.net/statistics/reports/ETH.pdf )
Deksissa ZM, Tesfamichael FA, Ferede HA (2015) Prevalence and factors associated with VIA positive result among clients screened at family guidance association of Ethiopia, south west area office, Jimma model clinic, Jimma, Ethiopia 2013: a cross-sectional study. BMC Res Notes 8:618
Megbaru S (2015) Trends of cervical cancer in Ethiopia. Gynecol Obstet 5(103):1
Tsehay B, Afework M (2020) Precancerous lesions of the cervix and its determinants among Ethiopian women: systematic review and meta-analysis. PLoS ONE 15(10):e0240353
Derbie A, Daniel M, Mezgebu Y, BIadgelgne F (2019) Magnitude of cervical lesions and its associated factors using visual inspection with acetic acid (VIA) at a referral hospital in Ethiopia. Ethiop Med J 57(2):1
Hailu A, Mariam DH (2013) Patient side cost and its predictors for cervical cancer in Ethiopia: a cross sectional hospital based study. BMC Cancer 13(1):69
Hailu A (2013) Patient cost of cervical cancer “immense” in Ethiopia. PharmacoEcon Outcomes News 674(1):7–7
Hagos A, Yitayal M, Kebede A, Debie A (2020) Economic burden and predictors of cost variability among adult cancer patients at comprehensive specialized hospitals in West Amhara, Northwest Ethiopia, 2019. Cancer Manag Res 12:11793–11802
Derbie A, Mekonnen D, Misgan E, Alemu YM, Woldeamanuel Y, Abebe T (2021) Low level of knowledge about cervical cancer among Ethiopian women: a systematic review and meta-analysis. Infect Agent Cancer 16(1):11
Mesafint Z, Berhane Y, Desalegn D (2018) Health seeking behavior of patients diagnosed with cervical cancer in Addis Ababa, Ethiopia. Ethiop J Health Sci 28(2):111–116
Getahun F, Addissie A, Negash S, Gebremichael G (2019) Assessment of cervical cancer services and cervical cancer related knowledge of health service providers in public health facilities in Addis Ababa, Ethiopia. BMC Res Notes 12(1):675
Begoihn M, Mathewos A, Aynalem A, Wondemagegnehu T, Moelle U, Gizaw M, Wienke A, Thomssen C, Worku D, Addissie A et al (2019) Cervical cancer in Ethiopia—predictors of advanced stage and prolonged time to diagnosis. Infect Agents Cancer 14(1):36
Kassie AM, Abate BB, Kassaw MW, Aragie TG, Geleta BA, Shiferaw WS (2020) Impact of knowledge and attitude on the utilization rate of cervical cancer screening tests among Ethiopian women: a systematic review and meta-analysis. PLoS ONE 15(12):e0239927
Molecular epidemiology of human papillomavirus in north and central part of Ethiopia ( http://etd.aau.edu.et/handle/123456789/14079 )
Abu SH, Woldehanna BT, Nida ET, Tilahun AW, Gebremariam MY, Sisay MM (2020) The role of health education on cervical cancer screening uptake at selected health centers in Addis Ababa. PLoS ONE 15(10):e0239580
Agide FD, Garmaroudi G, Sadeghi R, Shakibazadeh E, Yaseri M, Koricha ZB, Tigabu BM (2018) A systematic review of the effectiveness of health education interventions to increase cervical cancer screening uptake. Eur J Pub Health 28(6):1156–1162
Dias TC, Longatto-Filho A, Campanella NC (2020) Human papillomavirus genotyping as a tool for cervical cancer prevention: from commercially available human papillomavirus DNA test to next-generation sequencing. Future Sci OA 6(9):603
Münger K, Baldwin A, Edwards KM, Hayakawa H, Nguyen CL, Owens M, Grace M, Huh K (2004) Mechanisms of human papillomavirus-induced oncogenesis. J Virol 78(21):11451–11460
Williams VM, Filippova M, Soto U, Duerksen-Hughes PJ (2011) HPV-DNA integration and carcinogenesis: putative roles for inflammation and oxidative stress. Futur Virol 6(1):45–57
Kajitani N, Satsuka A, Kawate A, Sakai H (2012) Productive lifecycle of human papillomaviruses that depends upon squamous epithelial differentiation. Front Microbiol 3:152
Narisawa-Saito M, Kiyono T (2007) Basic mechanisms of high-risk human papillomavirus-induced carcinogenesis: roles of E6 and E7 proteins. Cancer Sci 98(10):1505–1511
Harald zur Hausen’s experiments on human papillomavirus causing cervical cancer (1976–1987): embryo project encyclopedia (2017-03-09) ( https://embryo.asu.edu/pages/harald-zur-hausens-experiments-human-papillomavirus-causing-cervical-cancer-1976-1987 )
Bouvard V, Baan R, Straif K, Grosse Y, Secretan B, El Ghissassi F, Benbrahim-Tallaa L, Guha N, Freeman C, Galichet L et al (2009) A review of human carcinogens—Part B biological agents. Lancet Oncol 10(4):321–322
Zhai L, Tumban E (2016) Gardasil-9: a global survey of projected efficacy. Antivir Res 130:101–109
Derbie A, Mekonnen D, Nibret E, Maier M, Woldeamanuel Y, Abebe T (2022) Human papillomavirus genetype distribution in Ethiopia: an updated systematic review. Virol J 19:3
Teka B, Gizaw M, Ruddies F, Addissie A, Chanyalew Z, Skof AS, Thies S, Mihret A, Kantelhardt EJ, Kaufmann AM et al (2021) Population-based human papillomavirus infection and genotype distribution among women in rural areas of South Central Ethiopia. Int J Cancer 148(3):723–730
Bruni L, Diaz M, Castellsagué X, Ferrer E, Bosch F, de Sanjosé S (2010) Cervical human papillomavirus prevalence in 5 continents: meta-analysis of 1 million women with normal cytological findings. J Infect Dis 202:1789–1799. https://doi.org/10.1086/657321
Pimenoff N, Tous S, Benavente Y, Alemany L, Quint W, Bosch F, Bravo G, Sanjosé S (2019) Distinct geographic clustering of oncogenic human papillomaviruses multiple infections in cervical cancers: results from a worldwide cross-sectional study. Int J Cancer 144:2478–2488. https://doi.org/10.1002/ijc.31964
Sanjose S, Quint G, Alemany L, Geraets T, Klaustermeier E, Lloveras B et al (2010) Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study. Lancet Oncol 11:1048–1056. https://doi.org/10.1016/S1470-2045(10)70230-8
Leto M, Santos Junior GF, Porro AM, Tomimori J (2011) Human papillomavirus infection: etiopathogenesis, molecular biology and clinical manifestations. An Bras Dermatol 86(2):306–317
García DA, Cid-Arregui A, Schmitt M, Castillo M, Briceño I, Aristizábal FA (2011) Highly sensitive detection and genotyping of hpv by pcr multiplex and luminex technology in a cohort of colombian women with abnormal cytology. Open Virol J 5:70–79
Pimple S, Mishra G, Shastri S (2016) Global strategies for cervical cancer prevention. Curr Opin Obstet Gynecol 28(1):4–10
Sahasrabuddhe VV, Luhn P, Wentzensen N (2011) Human papillomavirus and cervical cancer: biomarkers for improved prevention efforts. Future Microbiol 6(9):1083–1098
Tian Q, Li Y, Wang F, Xu J, Shen Y, Ye F, Wang X, Cheng X, Chen Y, Wan X et al (2014) MicroRNA Detection in Cervical Exfoliated Cells as a Triage for Human Papillomavirus-Positive Women. J Natl Cancer Inst. https://doi.org/10.1093/jnci/dju241
Wang HY, Lee D, Park S, Kim G, Kim S, Han L, Yubo R, Li Y, Park KH, Lee H (2015) Diagnostic performance of HPV E6/E7 mRNA and HPV DNA assays for the detection and screening of oncogenic human papillomavirus infection among woman with cervical lesions in China. Asian Pac J Cancer Prev 16(17):7633–7640
Cuschieri K, Wentzensen N (2008) Human papillomavirus mRNA and p16 detection as biomarkers for the improved diagnosis of cervical neoplasia. Cancer Epidemiol Biomark Prev 17(10):2536–2545
WHO (2015) ICO centre on HPV and cancer (HPV information centre). human papillomavirus and related diseases report
Sankaranarayanan R, Anorlu R, Sangwa-Lugoma G, Denny LA (2013) Infrastructure requirements for human papillomavirus vaccination and cervical cancer screening in sub-Saharan Africa. Vaccine 29(31):066
Tadesse SK (2015) Preventive mechanisms and treatment of cervical cancer in Ethiopia. Gynecol Obstet. https://doi.org/10.4172/2161-0932.S3:101
Louie KS, de Sanjose S, Mayaud P (2009) Epidemiology and prevention of human papillomavirus and cervical cancer in sub-Saharan Africa: a comprehensive review. Trop Med Int Health 14(10):1287–1302
WHO guidelines for screening and treatment of precancerous lesions for cervical cancer prevention. ( https://apps.who.int/iris/bitstream/handle/10665/94830/9789241548694_eng.pdf )
Eshete M, Abdulwuhab Atta M, Yeshita HY (2020) Cervical cancer screening acceptance among women in Dabat District, Northwest Ethiopia, 2017: an institution-based cross-sectional study. Obstet Gynecol Int 2020:2805936
Ruddies F, Gizaw M, Teka B, Thies S, Wienke A, Kaufmann AM, Abebe T, Addissie A, Kantelhardt EJ (2020) Cervical cancer screening in rural Ethiopia: a cross-sectional knowledge, attitude and practice study. BMC Cancer 20(1):563
Getachew S, Getachew E, Gizaw M, Ayele W, Addissie A, Kantelhardt EJ (2019) Cervical cancer screening knowledge and barriers among women in Addis Ababa, Ethiopia. PLoS ONE 14(5):e0216522
Bayu H, Berhe Y, Mulat A, Alemu A (2016) Cervical cancer screening service uptake and associated factors among age eligible women in mekelle zone, Northern Ethiopia, 2015: a community based study using health belief model. PLoS ONE 11(3):e0149908
Nigussie T, Admassu B, Nigussie A (2019) Cervical cancer screening service utilization and associated factors among age-eligible women in Jimma town using health belief model, South West Ethiopia. BMC Womens Health 19(1):127
Assefa AA, Astawesegn FH, Eshetu B (2019) Cervical cancer screening service utilization and associated factors among HIV positive women attending adult ART clinic in public health facilities, Hawassa town, Ethiopia: a cross-sectional study. BMC Health Serv Res 19(1):847
Dessalegn Mekonnen B (2020) Cervical cancer screening uptake and associated factors among HIV-positive women in ethiopia: a systematic review and meta-analysis. Adv Prev Med 2020:7071925
Ayenew AA, Zewdu BF, Nigussie AA (2020) Uptake of cervical cancer screening service and associated factors among age-eligible women in Ethiopia: systematic review and meta-analysis. Infect Agent Cancer 15(1):67
Wondimu YT (2015) cervical cancer: assessment of diagnosis and treatment facilities in public health institutions in addis ababa, ethiopia. Ethiop Med J 53(2):65–74
Vänskä S, Luostarinen T, Baussano I, Apter D, Eriksson T, Natunen K et al (2020) Vaccination with moderate coverage eradicates oncogenic human papillomaviruses if a gender-neutral strategy is applied. J Infect Dis. https://doi.org/10.1093/infdis/jiaa099
Lehtinen M, Luostarinen T, Vänskä S, Söderlund-Strand A, Eriksson T, Natunen K et al (2018) Gender-neutral vaccination provides improved control of human papillomavirus types 18/31/33/35 through herd immunity: results of a community randomized trial (III). Int J Cancer 142(5):949–958. https://doi.org/10.1002/ijc.31119
Download references
Acknowledgments
We would like to thank Bahir Dar and Addis Ababa Universities and CDT-Africa for the provided opportunity to undertake this review.
We received no funds for this particular review.
Author information
Authors and affiliations.
Department of Medical Microbiology, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
Awoke Derbie & Daniel Mekonnen
Centre for Innovative Drug Development and Therapeutic Trials for Africa (CDT-Africa), Addis Ababa University, Addis Ababa, Ethiopia
Awoke Derbie & Yimtubezinash Woldeamanuel
Department of Health Biotechnology, Biotechnology Research Institute, Bahir Dar University, Bahir Dar, Ethiopia
Department of Medical Microbiology, Immunology and Parasitology, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
Awoke Derbie, Yimtubezinash Woldeamanuel & Tamrat Abebe
Department of Biology, College of Science, Bahir Dar University, Bahir Dar, Ethiopia
Endalkachew Nibret
Department of Gynecology and Obstetrics, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
Eyaya Misgan
Department of Diagnostics, Institute of Virology, Leipzig University Hospital, Leipzig, Germany
Melanie Maier
You can also search for this author in PubMed Google Scholar
Contributions
AD and TA conceived the review topic and objectives. AD, DM and EM participated in the study selection and write-up. EN, MM, YW and TA reviewed the manuscript critically for its scientific content. All authors reviewed and approved the manuscript.
Corresponding author
Correspondence to Awoke Derbie .
Ethics declarations
Competing interest.
Authors declare that they have no competing interest.
Ethical approval
Not applicable in this section.
Consent to participate
Consent for publication, additional information, publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Derbie, A., Mekonnen, D., Nibret, E. et al. Cervical cancer in Ethiopia: a review of the literature. Cancer Causes Control 34 , 1–11 (2023). https://doi.org/10.1007/s10552-022-01638-y
Download citation
Received : 04 January 2022
Accepted : 26 September 2022
Published : 15 October 2022
Issue Date : January 2023
DOI : https://doi.org/10.1007/s10552-022-01638-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cervical cancer
- Human papillomavirus (HPV)
- Vaccination
- Cervical screening
- Find a journal
- Publish with us
- Track your research
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Knowledge and awareness of cervical cancer in Southwestern Ethiopia is lacking: A descriptive analysis
Atif saleem, alemayehu bekele, megan b fitzpatrick, eiman a mahmoud, athena w lin, h eduardo velasco, mona m rashed.
- Author information
- Article notes
- Copyright and License information
Competing Interests: The authors have declared that no competing interests exist.
* E-mail: [email protected]
Contributed equally.
Received 2019 Mar 26; Accepted 2019 Oct 23; Collection date 2019.
This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Cervical cancer remains the second most common cancer and cancer-related death among women in Ethiopia. This is the first study, to our knowledge, describing the demographic, and clinicopathologic characteristics of cervical cancer cases in a mainly rural, Southwestern Ethiopian population with a low literacy rate to provide data on the cervical cancer burden and help guide future prevention and intervention efforts.
A descriptive analysis of 154 cervical cancer cases at the Jimma University Teaching Hospital in Southwestern Ethiopia from January 2008 –December 2010 was performed. Demographic and clinical characteristics were obtained from patient questionnaires and cervical punch biopsies were histologically examined.
Of the 154 participants with a histopathologic diagnosis of cervical cancer, 95.36% had not heard of cervical cancer and 89.6% were locally advanced at the time of diagnosis. Moreover, 86.4% of participants were illiterate, and 62% lived in a rural area.
A majority of the 154 women with cervical cancer studied at the Jimma University Teaching Hospital in Southwestern Ethiopia were illiterate, had not heard of cervical cancer and had advanced disease at the time of diagnosis. Given the low rates of literacy and knowledge regarding cervical cancer in this population which has been shown to correlate with a decreased odds of undergoing screening, future interventions to address the cervical cancer burden here must include an effective educational component.
Introduction
Cervical cancer pathology and demographic data is lacking from Southwestern Ethiopia. The Jimma University Teaching Hospital (JUTH) is located in the city of Jimma which is 352 km southwest of Ethiopia’s capital city Addis Ababa and is unique in that it acts as the only teaching and referral hospital in the region, serving a population of 15 million people [ 1 ]. Moreover, Jimma is part of the Oromia state which has one of the highest poverty rates (74.9% of the population) and lowest literacy rates in the country (36% of all residents, with 17% of the female residents living in rural settings) [ 2 – 3 ]. Contributory data from this hospital is vital since every year, an estimated 7,095 women are diagnosed with cervical cancer and 4,732 deaths are due to the disease in Ethiopia—it is currently the second most common cause of female cancer deaths in Ethiopia, after breast cancer.
Infection with high-risk human papillomavirus (HPV) is the necessary cause of >99% of cervical cancer [ 4 ]. Other contributing factors include smoking, total fertility rate, and human immunodeficiency virus (HIV) infection [ 5 ]. The knowledge about cervical cancer in Ethiopia has been reported to range from 21.2% to 53.7%, with screening rates that ranged from 9.9% to 23.5%. Three of these four studies, however, took place in Northern Ethiopia [ 6 – 9 ]. Though there is not yet an organized cervical cancer education or screening program in Ethiopia, the ongoing dilemma remains how much the absence of such programs compared to a general lack of education or negative attitude towards cervical cancer contribute to the disease burden. Aweke et al. described that 34.8% of 583 survey respondents in Southern Ethiopia had a negative attitude pertaining to cervical cancer [ 7 ].
Materials and methods
Place of study.
The study took place at the Jimma University Teaching Hospital Departments of Obstetrics and Gynecology and Medical Laboratory Sciences and Pathology in Southwestern Ethiopia. This study, including the verbal/oral consent procedure, was approved by the Touro University California Institutional Review Board in the United States of America, by the Research and Publication Committee of the Faculty of Medical Sciences at Jimma University, by the Jimma University Ethics Review Committee and by the Jimma University Teaching Hospital Departments of Obstetrics and Gynecology and Medical Laboratory Sciences and Pathology in Ethiopia. Verbal/oral consent was only able to be obtained as opposed to written consent given that a significant proportion of the study population was not literate. The verbal/oral consent was recorded by the residents who were interviewing the subjects/performing the procedure onto individual survey sheets, which were then transcribed into a central document.
Study population
The study population included non-pregnant women voluntarily attending the Jimma University Teaching Hospital Department of Obstetrics and Gynecology outpatient clinic from January 2008 –December 2010 who had evidence of cervical lesions on initial pelvic examination. All of the participants voluntarily presented to the clinic and were willing to be screened; data was collected only after full informed oral consent for participating in the study was obtained.
Screening procedure
Data was collected by residents in the Department of Obstetrics and Gynecology who were informed regarding the study parameters and were in charge of the outpatient service on a rotation basis. All non-pregnant women with cervical lesions were invited to participate during the study time period. The patients were informed about the indications, contraindications, and alternative options of undergoing a cervical punch biopsy to recognize any cervical pathology. Oral consent was obtained from each case before the interview, punch biopsy procedure and data collection for participation in the study. Then each patient was interviewed using a standardized questionnaire ( S1 File ) to extract information regarding additional clinical features, sociodemographic characteristics, maternity history, and knowledge about cervical carcinoma, amongst others. Questionnaires were collected weekly and checked for adequacy—those with inadequate data (missing data or unrecognizable responses) were excluded. Pelvic examination was conducted to characterize the cervical lesion(s) and determine the clinical stage. Thorough speculum examination of the cervix was performed to describe any lesion(s) and subsequently a four quadrant punch biopsy of the cervix was taken. The biopsy material was preserved in 10% formaldehyde and submitted to the Department of Medical Laboratory Sciences and Pathology.
In the Department of Pathology the formalin fixed tissue was embedded in paraffin, sections were cut and subsequently stained as described. From each case, four microscopic slides were prepared–one remained in the Department of Pathology for clinical management and three were used for the current study. The slide used for clinical management was stained with hematoxylin and eosin (H&E) and diagnosed by a pathologist in the Department of Pathology according to the World Health Organization histological classification of tumors of the uterine cervix and this pathologic report was recorded and relayed to the physician specific to the case for clinical care. The H&E study slides were identified by the biopsy and code number assigned by the initial physician on the biopsy request sheet and questionnaire and were submitted for diagnosis to a pathologist from Touro University California who was blinded regarding the case for quality control. If there was disagreement in the reports between the slide used for clinical management and the second observer report, the slide was given to a third pathologist and the agreement of the two pathologists was taken as the gold standard report to be recorded.
Data analysis
Data was initially entered into Microsoft Excel after which it was coded and analyzed using STATA 15.0 software. Data cleaning was performed only in the form of eliminating missing data so as to improve accuracy, and descriptive statistics were subsequently used to summarize all variables.
A total of 240 women presented with various gynecological complaints to the outpatient clinic from January 2008 –December 2010. Eighty six women were excluded: 30 of these women had a diagnosis other than cervical cancer such as cervicitis or a cervical polyp but their remaining data was insufficient to analyze; the remaining 56 women were excluded due to an uninterpretable or equivocal biopsy. This left 154 cases to be analyzed and their subjective and objective clinical data is summarized in Tables 1 – 3 .
Table 1. Selected demographic and clinical features of 154 cervical cancer cases at the Jimma University Teaching Hospital, Ethiopia from January 2008—December 2010.
IQR: Interquartile range
Table 3. Selected objective clinical features of 154 cervical cancer cases at the Jimma University Teaching Hospital, Ethiopia from January 2008—December 2010.
Table 2. selected non-quantifiable demographic and clinical features of 154 cervical cancer cases at the jimma university teaching hospital, ethiopia from january 2008—december 2010..
a Other ethnicities included Shekicho, Gurage, Kulo, Yem, Kefa, Dawro, and Bench.
b Amongst those that admitted to using contraception, none practiced barrier contraception- only oral contraceptive pills or injectable contraceptives were used.
c Out of those that have heard of cervical cancer, all denied knowing the cause of it.
Demographic and clinical features
Cervical cancer is a unique cancer in that effective screening methods are known to prevent disease and associated mortality. Knowledge about the disease and preventive options are vital to effectively control the disease; however, we highlight in the current study that there is a considerable lack of knowledge and awareness regarding cervical cancer which is the second most common cause of cancer deaths in Ethiopia.
Knowledge about cervical cancer in Ethiopia has been reported to range from 21.2% to 53.7% [ 6 – 9 ], and Aweke et. Al described that 34.8% (n = 583) of survey respondents in Southern Ethiopia had a negative attitude pertaining to cervical cancer [ 7 ]. In our study a majority 144 women (95.36%) had not heard of cervical cancer compared to 138 out of 633 women (21.8%) who had not heard of it in a study done in Gondar town, northwest Ethiopia in 2010 [ 6 ]. In that cross-sectional survey, the literacy rate was 18.8%, whereas the rate was 86.4% in our current study. Moreover, a majority of our study participants lived in rural areas (62%) where access to television/radio and health professionals is limited- these were noted as the two most common sources for hearing about cervical cancer in the aforementioned study. The lack of knowledge regarding cervical cancer is of note since preventative efforts such as screening have been shown to reduce the risk of cervical cancer compared to no screening [ 10 ]; furthermore, a single-visit approach for cervical cancer screening in Ethiopia was described by Addis Tesfa in 2010 where visual inspection of the cervix with acetic acid wash (VIA) with subsequent cryotherapy of premalignant lesions was performed. One VIA at age 35 can reduce a woman’s lifetime risk of cervical cancer by 25% and if screened again at age 40 by 65% [ 11 ].
Cervical cancer educational strategies have been shown to improve screening in studies which targeted rural populations of sub-Saharan Africa [ 12 – 14 ]. Erku et al. describe that the odds of undergoing cervical cancer screening among women who had a comprehensive knowledge on cervical cancer and screening were 2.02 times higher than those who did not in a northwest Ethiopian population. In this study, a majority (87.7%) of the respondents had heard of cervical cancer. This is likely an overestimate since this study included a population of women living with HIV/acquired immunodeficiency syndrome (AIDS) which may have an increased level of awareness with more frequent healthcare visits [ 8 ].
In Ethiopia, currently there are approximately 25 cervical cancer screening centers that are providing visual inspection with acetic acid (VIA), however there is low participation in the community which is partly attributed to the lack of awareness regarding this disease [ 15 ]. Geremew et al describe that college and above educational status, knowing someone with cervical cancer, and having knowledge of cervical cancer were positively associated with favorable attitudes towards cervical cancer screening [ 16 ]; in the current study, a majority of the patients were illiterate and had decreased knowledge regarding cervical cancer which may explain the lack of screening in our specific population. The National Cancer Control Plan of Ethiopia headed by the Federal Ministry of Health Ethiopia plans a nation-wide scale up of the screening and treatment of cervical pre-cancerous lesions into over 800 health facilities [ 17 ]. The mean age at diagnosis of cervical cancer in the United States has been shown to be 48 years and in our study from Ethiopia it was 45 years [ 18 ]. Our study differs in that there is no data on prior screening which may have decreased the age at diagnosis and if so, could be attributed to a possible faster progression from HPV to cervical cancer secondary to HIV co-infection or other synergistic risk factors, particularly in the absence of a cervical cancer screening program. Established risk factors for most cervical cancer include: early onset of sexual activity, multiple sexual partners, immunosuppression, increasing parity, low socioeconomic status and oral contraceptive use [ 5 ].
A qualitative study of 198 patients with cervical cancer from Tikur Anbessa Hospital in Addis Ababa, Ethiopia in 2013 [ 19 ] is compared to our study at JUTH in Table 4 . The mean age at first sexual intercourse in southwestern Ethiopia has previously been shown to be 17.07 years (+/- 2.12) in a group of 405 young women where cervical lesions were not studied [ 20 ]. Our data of cervical cancer cases shows the mean age at first sexual intercourse to be 15.83 years (+/- 2.08) and the mean age from the Tikbur Anbessa study is 16.5 years which may be explained by the cultural practice of marriage at a younger age in these selected populations.
Table 4. Comparison of data pertinent to selected risk factors for cervical cancer from Jimma University Teaching Hospital in southwestern Ethiopia (January 2008—December 2010) and Tikbur Anbessa Hospital in Addis Ababa, Ethiopia (April 2013) [ 19 ] from women with a diagnosis of cervical cancer to that of representative women in Ethiopia (where cervical lesions were not necessarily studied).
a (Out of 198 respondents, 52.3% responded 1, 33% responded 2 and 29% responded 3 or more).
Prior studies found that the mean number of sexual partners in Ethiopia for women is approximately 1.5 (cervical lesions not specified) compared to our study which is 2.9 [ 21 – 22 ] and an increased number of sexual partners raises the probability of becoming infected with HPV. The total fertility rate is estimated to be 4.8 children per woman in Ethiopia (cervical lesions not specified) compared to our study which is 6.27 per woman. The proposed mechanism for higher parity as a risk factor for cervical cancer include increased estrogen exposure during pregnancy, persistence of the transformation zone on the ectocervix in multiparous women, and cervical tissue damage during vaginal deliveries [ 22 ].
Hormonal steroids (such as those in oral contraceptive pills) have been shown to activate enhancer elements in the upstream regulatory region of the HPV type 16 viral genome which is one proposed mechanism for the increased risk of cervical cancer [ 23 ]. Out of the 35 women (23.33%) in our study used contraception, none practiced barrier contraception. The majority of these 35 women (80%) used oral contraceptive pills which have been shown to increase the cumulative incidence of invasive cervical cancer by age 50 from 7.3 to 8.3 per 1000 in developing countries [ 24 ].
This study took place during the rapid expansion phase of HIV/AIDS services in Ethiopia where the number of patients on antiretroviral therapy (ART) increased from 900 at the beginning of 2005 to over 150,000 by June 2008 [ 25 ]. Despite this increase in ART use, the frequency of cervical cancer cases in Ethiopia has increased from 2005 until present, with a yearly increment from 1997–2012 except in 1999 and 2009 [ 26 ]. This increase may, however, be attributed to increased awareness, screening and subsequent diagnosis. In our study, a majority of women presented at stage IIB followed by stage IIIA at the time of diagnosis and the general trends in Ethiopia at that time remained at presenting at stage IIIB being the most frequent, and secondly stage IIB ( Table 5 ).
Table 5. Clinical stages of cervical carcinoma cases at presentation.
Histopathologic classification.
The majority of cervical cancers in the United States are squamous cell carcinoma (69%) followed by adenocarcinoma (25%) [ 27 ]. Histopathologic subtype classification in a study of 598 cervical cancer cases in Nigeria and 2,930 cervical cancer cases in South Africa demonstrated squamous cell carcinoma as the most common type as was shown in 92.3% and greater than 80% of cases, respectively [ 28 – 29 ]. In the United States, other non-squamous cervical cancers have been observed in the following frequencies: adenosquamous carcinomas represent 20%-30% of all adenocarcinomas of the cervix and small cell carcinomas represent 0.5%-5% of all invasive cervical cancers. In our study, approximately 91% of the cervical cancer cases were squamous cell carcinomas (including keratinizing, non-keratinizing and basaloid subtypes), 5.84% were small cell carcinomas, 2.59% were adenocarcinomas, and 0.64% were adenosquamous carcinomas. The squamous cell carcinoma frequency was similar to that observed in prior studies; however, an increased frequency of small cell carcinomas over adenocarcinomas was also noted in our study. It has been shown that the keratinizing squamous cell carcinoma subtype is associated with a higher likelihood of advanced stage disease and a lower overall 5-year survival [ 30 ] and in our study we observed a 51.29% frequency of this subtype.
The HPV-18 genotype is more commonly associated with adenocarcinomas and small cell carcinomas of the cervix; however, the cases in this study were not subtyped. Few studies describing the high-risk HPV genotypes have been performed in Ethiopia out of which one study of 98 women with cervical dysplasia in Jimma showed that HPV-18 was detected in 8.2% of the 67.1% of HPV DNA positive samples [ 31 ]. Based on other studies, HPV type 18 is detected in 18.2% of cervical cancer cases in Ethiopia [ 32 ].
A population based study from 1988–2004 of 6,853 women with squamous cell carcinoma found that keratinizing squamous cell carcinoma of the cervix may be less radiosensitive and associated with shorter overall survival than non-keratinizing squamous cell carcinoma [ 30 ]. In our study, a majority of women presented with locally advanced cervical cancer (89.6%, Table 5 ), whereas approximately 54.9–58.8% of patients were diagnosed at a late stage in a California database from the United States [ 33 ], as a means of comparison to a high-income country with an established screening program in place. We believe the majority of women in our study presented with locally advanced lesions not entirely due to an intrinsic pathogenetic difference, but because of lack of a cervical screening program in Ethiopia, decreased knowledge about cervical cancer, inability to attend health clinics due to cost and travel expenditure, and increased exposure to risk factors.
Limitations, future directions and recommendations
Our study did not perform laboratory confirmation of HPV or HIV infection, or test for co-infections with other sexually transmitted infections. Recall bias may have affected the demographic data since it was procured by a survey. Future directions include measuring survival outcomes after intervention for cervical cancer and studying the effectiveness of cervical cancer screening after education. Based on our data, in this specific population of Ethiopian women we recommend promoting an educational initiative about cervical cancer among Ethiopian women given that improved knowledge regarding the disease has been shown to increase screening and decrease cervical cancer rates.
Conclusions
Most of the 154 women with cervical cancer studied at the JUTH in southwestern Ethiopia were illiterate, had not heard of cervical cancer, had advanced disease at the time of diagnosis and had microscopically confirmed squamous cell carcinomas. The low rates of literacy and knowledge regarding cervical cancer in this population were also associated with lower screening rates. Future interventions to address the cervical cancer burden in Ethiopia should include an effective educational component which has been shown to increase screening rates and ultimately decrease the cervical cancer incidence.
Supporting information
Each patient was orally interviewed by residents using this standardized questionnaire who then input the information accordingly. The histopathology data (Section IV) was completed by a pathologist.
Acknowledgments
We would like to acknowledge the Jimma University Teaching Hospital and the Global Physicians Corps for their technical support in this study, and to the Touro University California Institutional Review Board in the United States of America, the Research and Publication Committee of the Faculty of Medical Sciences at Jimma University, the Jimma University Ethics Review Committee and the Jimma University Teaching Hospital Departments of Obstetrics and Gynecology and Medical Laboratory Sciences and Pathology in Ethiopia for their approval and permission to perform this study. We would also like to acknowledge all of the physicians/trainees/staff who assisted in data collection and to all of the study participants who provided this vital data in an overall effort to study and reduce the morbidity/mortality attributed to cervical cancer.
Data Availability
The data underlying the results presented in the study has been de-identified and is available from: Inter-university Consortium for Political and Social Research [distributor], 2019-10-04. https://doi.org/10.3886/E112185V1 .
Funding Statement
This study was funded in terms of the materials (questionnaires, histopathological materials including microscopic slides/staining materials) by the Jimma University Teaching Hospital and by the Global Physicians Corps ( http://globalphysicians.org/ ).
- 1. Jimma University Specialized Hospital: Historical Background: https://www.ju.edu.et/jimma-university-specialized-hospital-jush . Cited 20 March 2019.
- 2. Oxford Poverty and Human Development Initiative (OPHI) www.ophi.org.uk . Oxford Department of International Development. Queen Elizabeth House, University of Oxford. OPHI Country Briefing 2017: Ethiopia. Global Multidimensional Poverty Index (MPI).
- 3. Adugna A. Oromiya: Demography and Health; 2017 [cited 2019 March 5]. http://www.ethiodemographyandhealth.org/Oromia.html .
- 4. Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189(1):12–9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 5. International Collaboration of Epidemiological Studies of Cervical Cancer. Comparison of risk factors for invasive squamous cell carcinoma and adenocarcinoma of the cervix: collaborative reanalysis of individual data on 8,097 women with squamous cell carcinoma and 1,374 women with adenocarcinoma from 12 epidemiological studies. Int J Cancer. 2007;120(4):885–91. 10.1002/ijc.22357 [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Getahun F, Mazengia F, Abuhay M, Birhanu Z. Comprehensive knowledge about cervical cancer is low among women in Northwest Ethiopia. BMC cancer. 2013. December;13(1):2. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Aweke YH, Ayanto SY, Ersado TL. Knowledge, attitude and practice for cervical cancer prevention and control among women of childbearing age in Hossana Town Hadiya zone, Southern Ethiopia: Community-based cross-sectional study. PLoS One. 2017. July 25;12(7):e0181415 10.1371/journal.pone.0181415 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 8. Erku DA, Netere AK, Mersha AG, Abebe SA, Mekuria AB, Belachew SA. Comprehensive knowledge and uptake of cervical cancer screening is low among women living with HIV/AIDS in Northwest Ethiopia. Gynecol Oncol Res Pract. 2017. December 19;4:20 10.1186/s40661-017-0057-6 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 9. Mitiku I, Tefera F. Knowledge about cervical cancer and associated factors among 15–49 year old women in Dessie Town, Northeast Ethiopia. PLoS One. 2016. September 30;11(9):e0163136 10.1371/journal.pone.0163136 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 10. Peirson L, Fitzpatrick-Lewis D, Ciliska D, Warren R. Screening for cervical cancer: a systematic review and meta-analysis. Systematic reviews. 2013. December;2(1):35. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 11. Shiferaw N, Salvador-Davila G, Kassahun K, Brooks MI, Weldegebreal T, Tilahun Y, et al. The single-visit approach as a cervical cancer prevention strategy among women with HIV in Ethiopia: successes and lessons learned. Global Health: Science and Practice. 2016. March 21;4(1):87–98. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 12. Abiodun OA, Olu-Abiodun OO, Sotunsa JO, Oluwole FA. Impact of health education intervention on knowledge and perception of cervical cancer and cervical screening uptake among adult women in rural communities in Nigeria. BMC public health. 2014. December;14(1):814. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 13. Chigbu CO, Onyebuchi AK, Onyeka TC, Odugu BU, Dim CC. The impact of community health educators on uptake of cervical and breast cancer prevention services in Nigeria. International Journal of Gynecology & Obstetrics. 2017. June 1;137(3):319–24. [ DOI ] [ PubMed ] [ Google Scholar ]
- 14. Johnson LG, Armstrong A, Joyce CM, Teitelman AM, Buttenheim AM. Implementation strategies to improve cervical cancer prevention in sub-Saharan Africa: a systematic review. Implementation Science. 2018. December;13(1):28 10.1186/s13012-018-0718-9 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 15. Teame H, Addissie A, Ayele W, Hirpa S, Gebremariam A, Gebreheat G, et al. Factors associated with cervical precancerous lesions among women screened for cervical cancer in Addis Ababa, Ethiopia: A case control study. PloS one. 2018. January 19;13(1):e0191506 10.1371/journal.pone.0191506 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 16. Geremew AB, Gelagay AA, Azale T. Comprehensive knowledge on cervical cancer, attitude towards its screening and associated factors among women aged 30–49 years in Finote Selam town, northwest Ethiopia. Reproductive health. 2018. December;15(1):29 10.1186/s12978-018-0471-1 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 17. Federal Ministry of Health Ethiopia. National Cancer Control Plan 2015/2016-2019/2020. Addis Ababa, Ethiopia: Federal Ministry of Health; 2015. [ Google Scholar ]
- 18. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet‐Tieulent J, Jemal A. Global cancer statistics, 2012. CA: a cancer journal for clinicians. 2015. March;65(2):87–108. [ DOI ] [ PubMed ] [ Google Scholar ]
- 19. Tadesse SK. Socio-economic and cultural vulnerabilities to cervical cancer and challenges faced by patients attending care at Tikur Anbessa Hospital: a cross sectional and qualitative study. BMC women’s health. 2015. December;15(1):75. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 20. Tilahun M, Ayele G. Factors associated with age at first sexual initiation among youths in Gamo Gofa, south west Ethiopia: a cross sectional study. BMC Public Health. 2013. December;13(1):622. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 21. CSA-Ethiopia IC. International: Ethiopia Demographic and Health Survey 2011. 2012. Maryland, USA: Central Statistical Agency of Ethiopia and ICF International Addis Ababa, Ethiopia and Calverton; 2011. [ Google Scholar ]
- 22. Jensen KE, Schmiedel S, Norrild B, Frederiksen K, Iftner T, Kjaer SK. Parity as a cofactor for high-grade cervical disease among women with persistent human papillomavirus infection: a 13-year follow-up. British journal of cancer. 2013. January;108(1):234 10.1038/bjc.2012.513 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 23. Moodley M, Moodley J, Chetty R, Herrington CS. The role of steroid contraceptive hormones in the pathogenesis of invasive cervical cancer: a review. International Journal of Gynecological Cancer. 2003. March;13(2):103–10. 10.1046/j.1525-1438.2003.13030.x [ DOI ] [ PubMed ] [ Google Scholar ]
- 24. International Collaboration of Epidemiological Studies of Cervical Cancer. Cervical cancer and hormonal contraceptives: collaborative reanalysis of individual data for 16 573 women with cervical cancer and 35 509 women without cervical cancer from 24 epidemiological studies. The Lancet. 2007. November 10;370(9599):1609–21. [ DOI ] [ PubMed ] [ Google Scholar ]
- 25. Assefa Y, Jerene D, Lulseged S, Ooms G, Van Damme W. Rapid scale-up of antiretroviral treatment in Ethiopia: successes and system-wide effects. PLoS medicine. 2009. April 28;6(4):e1000056 10.1371/journal.pmed.1000056 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 26. Abate SM. Trends of cervical cancer in Ethiopia. Gynecol Obstet (Sunnyvale). 2015;5(103):2161–0932. [ Google Scholar ]
- 27. Rates RS. SEER cancer statistics review 1975–2004.
- 28. Olu-Eddo AN, Ekanem VJ, Umannah I, Onakevhor J. A 20 year histopathological study of cancer of the cervix in Nigerians. Nigerian quarterly journal of hospital medicine. 2011;21(2):149–53. [ PubMed ] [ Google Scholar ]
- 29. Moodley M, Moodley K. Trends of histopathology of cervical cancer among women in Durban, South Africa. European journal of gynaecological oncology. 2009;30(2):145–50. [ PubMed ] [ Google Scholar ]
- 30. Kumar S, Shah JP, Bryant CS, Imudia AN, Ali-Fehmi R, Malone JM Jr, et al. Prognostic significance of keratinization in squamous cell cancer of uterine cervix: a population based study. Arch Gynecol Obstet. 2009. July;280(1):25–32. 10.1007/s00404-008-0851-9 [ DOI ] [ PubMed ] [ Google Scholar ]
- 31. Bekele A, Baay M, Mekonnen Z, Suleman S, Chatterjee S. Human papillomavirus type distribution among women with cervical pathology–a study over 4 years at Jimma Hospital, southwest Ethiopia. Tropical Medicine & International Health. 2010. August;15(8):890–3. [ DOI ] [ PubMed ] [ Google Scholar ]
- 32. Bruni L, Barrionuevo-Rosas L, Albero G, Serrano B, Mena M, Gómez D, et al. ICO Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in the World. Summary Report 7 October 2016.
- 33. Maguire FB, Chen Y, Morris CR, Parikh-Patel A, Kizer KW. Heat Maps: Trends in Late Stage Diagnoses of Screenable Cancers in California Counties, 1988–2013. Sacramento, CA: California Cancer Reporting and Epidemiologic Surveillance Program, Institute for Population Health Improvement, University of California Davis, June 2016. [ Google Scholar ]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data availability statement.
- View on publisher site
- PDF (394.4 KB)
- Collections

Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Cervical cancer screening utilization and predictors among eligible women in Ethiopia: A systematic review and meta-analysis
Melaku desta, temesgen getaneh, bewuket yeserah, yichalem worku, tewodros eshete, molla yigzaw birhanu, getachew mullu kassa, fentahun adane, yordanos gizachew yeshitila.
- Author information
- Article notes
- Copyright and License information
Competing Interests: The authors have declared that no competing interests exist.
* E-mail: [email protected]
Received 2020 Jul 23; Accepted 2021 Oct 18; Collection date 2021.
This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Despite a remarkable progress in the reduction of global rate of maternal mortality, cervical cancer has been identified as the leading cause of maternal morbidity and mortality, particularly in sub-Saharan African countries. The uptake of cervical cancer screening service has been consistently shown to be effective in reducing the incidence rate and mortality from cervical cancer. Despite this, there are limited studies in Ethiopia that were conducted to assess the uptake of cervical cancer screening and its predictors, and these studies showed inconsistent and inconclusive findings. Therefore, this systematic review and meta-analysis was conducted to estimate the pooled cervical cancer screening utilization and its predictors among eligible women in Ethiopia.
Methods and findings
Databases like PubMed, Web of Science, SCOPUS, CINAHL, Psychinfo, Google Scholar, Science Direct, and the Cochrane Library were systematically searched. All observational studies reporting cervical cancer screening utilization and/ or its predictors in Ethiopia were included. Two authors independently extracted all necessary data using a standardized data extraction format. Quality assessment criteria for prevalence studies were adapted from the Newcastle Ottawa quality assessment scale. The Cochrane Q test statistics and I 2 test were used to assess the heterogeneity of studies. A random effects model of analysis was used to estimate the pooled prevalence of cervical cancer screening utilization and factors associated with it with the 95% confidence intervals (CIs). From 850 potentially relevant articles, twenty-five studies with a total of 18,067 eligible women were included in this study. The pooled national cervical cancer screening utilization was 14.79% (95% CI: 11.75, 17.83). The highest utilization of cervical cancer screening (18.59%) was observed in Southern Nations Nationalities and Peoples’ region (SNNPR), and lowest was in Amhara region (13.62%). The sub-group analysis showed that the pooled cervical cancer screening was highest among HIV positive women (20.71%). This meta-analysis also showed that absence of women’s formal education reduces cervical cancer screening utilization by 67% [POR = 0.33, 95% CI: 0.23, 0.46]. Women who had good knowledge towards cervical screening [POR = 3.01, 95%CI: 2.2.6, 4.00], perceived susceptibility to cervical cancer [POR = 4.9, 95% CI: 3.67, 6.54], severity to cervical cancer [POR = 6.57, 95% CI: 3.99, 10.8] and those with a history of sexually transmitted infections (STIs) [POR = 5.39, 95% CI: 1.41, 20.58] were more likely to utilize cervical cancer screening. Additionally, the major barriers of cervical cancer screening utilization were considering oneself as healthy (48.97%) and lack of information on cervical cancer screening (34.34%).
Conclusions
This meta-analysis found that the percentage of cervical cancer screening among eligible women was much lower than the WHO recommendations. Only one in every seven women utilized cervical cancer screening in Ethiopia. There were significant variations in the cervical cancer screening based on geographical regions and characteristics of women. Educational status, knowledge towards cervical cancer screening, perceived susceptibility and severity to cervical cancer and history of STIs significantly increased the uptake of screening practice. Therefore, women empowerment, improving knowledge towards cervical cancer screening, enhancing perceived susceptibility and severity to cancer and identifying previous history of women are essential strategies to improve cervical cancer screening practice.
Despite a remarkable progress in the reduction of maternal mortality, cervical cancer is the second most commonly diagnosed cancer and the leading cause of cancer related death among African women [ 1 ]. There were approximately 236,000 deaths from cervical cancer worldwide and it was the most common cancer in east and middle Africa [ 2 , 3 ]. About 90% of cases and 85% of these deaths have occurred in Low and Middle-Income Countries (LMICs); the highest has occurred in Sub-Saharan Africa (SSA) and approximately 311,000 women died from cervical cancer [ 2 ]. The incidence, the death rate and morbidities associated with cervical cancer significantly varies across the world; higher in the developing nations compared to the developed countries [ 4 ]. The high burden of cervical cancer is mainly due to the early onset of sexual intercourse, multiple sexual partners, human immunodeficiency virus (HIV) infection, history of sexually transmitted infections (STIs), human papilloma virus (HPV) infection, cigarette smoking, limited resources for early detection and poor HPV vaccination coverage [ 5 , 6 ].
Almost all of the maternal deaths associated with cervical cancer could be prevented if early and effective interventions mechanisms to cervical cancer control were available to all women. In particular, a comprehensive approach such as prevention, early diagnosis, effective screening and treatment programmes of pre-cervical lesions are essential for prevention of cervical cancer [ 7 ]. Visual inspection with Acetic Acid (VIA) and Visual Inspection with Lugol’s Iodine (VILI) are commonly used in low-resource settings [ 6 ]. VIA combined with the immediate treatment of women who tested positive at the first visit was cost saving and was the next most effective strategy, with a 26% decrease in the incidence of CC, further reduce mortality due to CC. A large-cluster randomized trial from rural India showed that a single round of HPV screening could reduce the incidence and mortality from CC of approximately 50% [ 8 ].
The guidelines of the World Health Organization (WHO), the United States Preventive Services Task Force (USPSTF) and the American Cancer Society (ACS) recommends that all eligible women should have cervical cancer screening at least once every three years [ 9 ]. Ethiopia adopted WHO’s recommendation that woman aged 30 and above should begin screening for cervical cancer at least one to three years of age with a see- and -treat approach. However, sexually active and HIV-positive women (start screening at HIV diagnosis) are suggested to be screened every 3 years regardless of their age [ 10 ]. The prevalence of cervical cancer screening is much higher at the Western countries than SSA [ 11 , 12 ]; 85.0% in the United States, 78.6% in the United Kingdom [ 13 ], and ranges from 2% in Ethiopia, 6% in Kenya [ 14 ], to 8% in Nigeria [ 15 ]. The lower rate of cervical cancer screening programme at LMICs may be related to the complexity of the screening process and the common inherent barriers in the setting such as poverty, limited access to information, lack of knowledge of cervical cancer, lack of healthcare infrastructure required, lack of trained practitioners and the absence of sustained prevention programmes [ 16 ].
The government of Ethiopia launched a cervical cancer screening service and has given more emphasis on programs focusing on the early detection of cervical cancer using advocacy efforts by different stakeholders such as academia, professionals, media and partners. However, the prevalence of cervical cancer remains a major problem, and it is one of the leading causes of morbidity and mortality among women in the country [ 17 , 18 ]. Evidence show success of cervical screening initiatives depend on high participation of the target population, which in turn is determined by the women’s knowledge, perceptions, health orientations and other socio-cultural issues. It is also affected by factors including early marriage, early sexual practice, delivery of the first baby before the age of 20, multiple sexual partners and low socio economic status. Therefore, addressing the different barriers for poor utilization of cervical cancer screening is essential component of intervention. Although, there were previous pocket studies conducted on these issues in Ethiopia, the studies showed fragmented, inconsistent and inconclusive findings. Even the studies were fragmented in different specific population characteristics like among HIV positive women and reproductive age women. Therefore, this systematic review and meta-analysis aimed to estimate the pooled cervical cancer screening utilization and its predictors among all eligible women in Ethiopia. It also aimed to address the common barriers of cervical cancer screening.
Registration of systematic review, data sources and search strategies
The purpose of this systematic review and meta-analysis was to estimate the pooled utilization level of cervical cancer screening and its predictors among women of reproductive-aged in Ethiopia. The protocol has been registered with the International Prospective Register of Systematic Review (PROSPERO), the University of York Center for Reviews and Dissemination ( https://www.crd.york.ac.uk/ ), registration number CRD42019119626 . The findings of this review have been reported as recommended by the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA-P) 2009 statement checklist [ 19 ] ( S1 Table ). All published articles were searched from major international databases like PubMed, Cochrane Library, Psych Info, Scopus, CINAHL, Web of Science, Science Direct, Google Scholar and African Journals Online. Additionally, Google hand searches were used mainly for unpublished studies. A search was also made for the reference list of studies already identified in order to retrieve additional articles. The Population, Exposure, Comparison and Outcomes (PECO) search formula was used to retrieve articles.
All eligible women for cervical cancer screening Ethiopia were the population of interest for this study. The outcome of interest was the utilization of cervical cancer screening among women. The predictor variables of cervical cancer screening utilization included in this study were age of women, educational status, and occupational status, knowledge of cervical cancer screening, perceived susceptibility and severity to cervical cancer and history of sexually transmitted infections. Comparisons were defined for each predictor based on the reported reference group for each predictor in each respective variable.
For each of the selected components of PECO, electronic databases were searched using the keyword search and the medical subject heading [MeSH] words. The keywords include “utilization, uptake, cervical cancer, screening, and women of reproductive age as well as Ethiopia”. The search terms were combined by the Boolean operators "OR" and "AND. The specific searching detail in PubMed was putted in S1 Appendix .
Eligibility criteria and study selection
This review included studies that reported either the use of cervical cancer screening or the cervical cancer screening predictors in Ethiopia. All published and unpublished studies through April 7, 2020 and reported in English language were retrieved to assess eligibility for inclusion in this review. However, this review excluded studies that were case reports of populations, surveillance data (demographic health survey), and abstracts of conferences, articles without full access and the outcome of interest not reported. The article selection underwent several steps. Two reviewers (MD and TE) evaluated the retrieved articles for inclusion using their title, abstract and full text review. Any disagreement during the selection process between the reviewers was resolved by consensus. Full texts of selected articles were then evaluated using the prior eligibility. During the encounter of duplication; only the full-text article was retained.
Quality assessment and data collection
The Newcastle-Ottawa Scale (NOS) quality assessment tool was used to assess the quality of the included studies. The tool contains three components- selection of the study groups, comparability of the study groups, and ascertainment of exposure or outcome [ 20 ]. The main component of the tool was graded from five stars and mainly emphasized on the methodological quality of each primary study. The other component of the tool graded from two stars and mainly concerned with the comparability of each study. The last component of the tool was graded from three stars and was used to evaluate the results and statistical analysis of each original study. The NOS included three categorical criteria with a maximum score of 9 points. The quality of each study was assessed using the following score algorithms: ≥7 points were considered as “good”, 4 to 6 points were considered as “moderate”, and ≤ 3 point was considered as “poor” quality studies. In order to improve the validity of this systematic review result, only primary studies of fair to good quality have been included. The two reviewers (MD and TE) independently assessed articles for overall study quality and extracted data using a standardized data extraction format. The data extraction format included primary author, year of publication, region of the study, sample size, prevalence, and the selected predictors of cervical cancer screening utilization.
Publication bias and statistical analysis
The publication bias was assessed using the Egger’s [ 21 ] and Begg’s [ 22 ] tests with a p-value of less than 0.05. The I 2 statistic was used to assess heterogeneity between studies and a p-value of less than 0.05 was used to detect heterogeneity. As a result of the presence of heterogeneity, a random-effects model was used as a method of analysis [ 23 ]. Data were extracted in Microsoft Excel and exported to Stata version 11 for analysis. Subgroup analysis was conducted by geographic region, population’s characteristics and design or type of study. Moreover, a meta-regression model based on sample size and year of publication was used to identify the sources of random variations in the included studies. The effect of selected determinant variables was analyzed using separate categories of meta-analysis [ 24 ]. The findings of the meta-analysis were presented using forest plots and Odds Ratio (OR) with its 95% Confidence intervals (CI). In addition, we conducted a sensitivity analysis to assess whether the pooled prevalence estimates were influenced by individual studies.
Study identification and characteristics of included studies
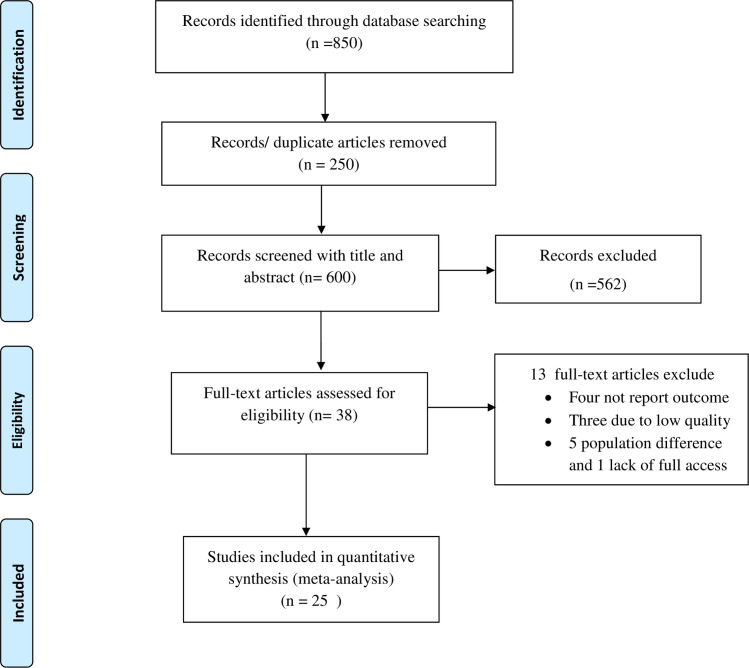
This systematic review and meta-analysis included both published and unpublished studies on the use of cervical cancer screening in Ethiopia. A total of 850 articles were found from the review. Of these, 250 duplicated records were removed and 581 articles were excluded by screening using their titles and abstracts. Subsequently, a total of 38 full-text papers were assessed for eligibility on the basis of the inclusion and exclusion criteria. Thus, four studies were excluded due to lack of the outcome of interest [ 25 – 30 ], three due to low quality [ 31 – 33 ], five due to difference in the study population [ 34 – 39 ] and only one study was excluded due to lack of access to the full text [ 40 ]. Finally, 25 studies were included in the final quantitative meta-analysis ( Fig 1 ).
Fig 1. PRISMA flow diagram of cervical cancer screening utilization in Ethiopia.
All of the included studies were cross-sectional. From this, twelve studies were facility- based cross sectional studies (FBCS) and thirteen were community- based cross-sectional studies (CBCS). The review was conducted among 18,067 women to estimate the pooled prevalence of cervical cancer screening. Publication of articles was between 2016 and 2020. The largest sample size was 5,823 women in a national level study [ 41 ] and the smallest sample was 250 women from a study conducted in Oromia region [ 42 ]. All studies were conducted in five geographic regions of Ethiopia. Four studies (16%) were from Addis Ababa [ 43 – 46 ], nine (36%) were from Amhara [ 47 – 55 ], four (16%) were from Southern Nations, Nationalities and Peoples Representative (SNNPR) [ 56 – 60 ], four (16%) were from Oromia [ 42 , 61 – 63 ], two (8%) were from Tigray [ 64 , 65 ], and the remaining one study [ 41 ] was a national- level study. Twelve studies were conducted among eligible women with no specific characteristics of their HIV status [ 44 , 47 ], five studies on HIV-positive women [ 43 , 48 , 53 , 61 , 63 ], four studies among healthcare workers [ 59 , 63 , 65 , 66 ] and the remaining one study [ 51 ] was conducted among women who were commercial sex workers ( Table 1 ).
Table 1. Characteristics of the included studies in the meta-analysis, Ethiopia.
AA: Addis Ababa; CSWs: Commercial sex workers.
CBCS: community based cross-sectional study; FBCS: facility based cross-sectional study.
Meta-analysis of cervical cancer screening utilization in Ethiopia
The highest cervical cancer screening utilization was observed in SNNPR, a study conducted at ART health facilities of Hawassa, 40% [ 57 ] and Wolayita hospitals, 22.9% [ 60 ]. Whereas, the lowest was 2.9% in a national level study [ 41 ] and 5.4% from a study conducted in Amhara region [ 54 ].
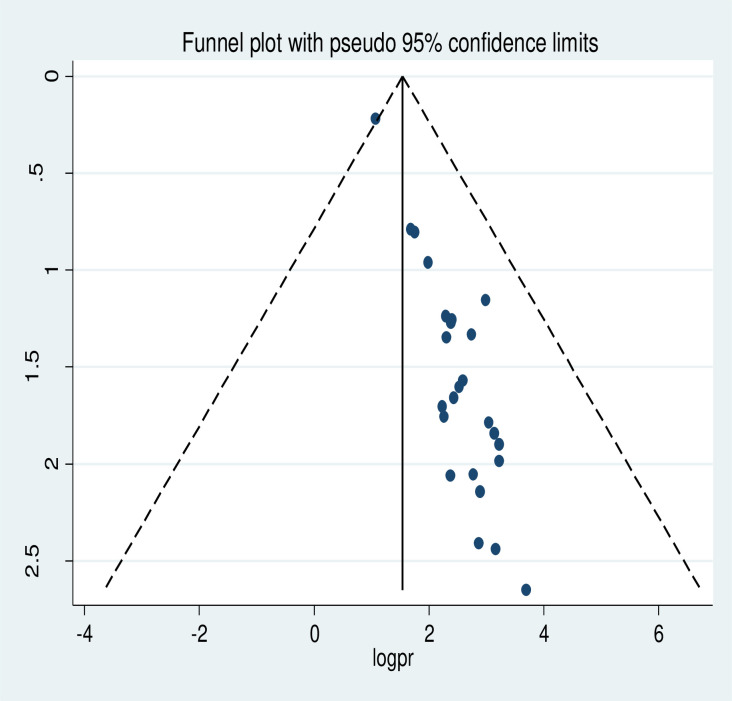
The meta-analysis of twenty-five studies showed that the pooled national level of cervical cancer screening utilization was 14.79% (95% CI: 11.75, 17.83). A random-effect model of analysis was used due to significant heterogeneity ( I 2 = 97.9%, p-value <0.05) ( Fig 2 ). Publication bias was assessed using Eggers test and it was statistically significant, p-value less than 0.0001. To account for publication bias, the duval and trimmed full analysis was performed. The univariate meta-regression model was also used to identify possible sources of heterogeneity using different covariates like year of publication and sample size. However, none of these variables were found to be statistically significant, p-value > 0.05. Moreover, the sensitivity analysis using a random-effects model showed that no single study had unduly influenced the overall estimate of the use of cervical cancer screening among Ethiopian women ( S1 Fig ). The funnel plot also showed that there was symmetrical distribution ( Fig 3 ).
Fig 2. The pooled utilization of cervical cancer screening among women in Ethiopia.
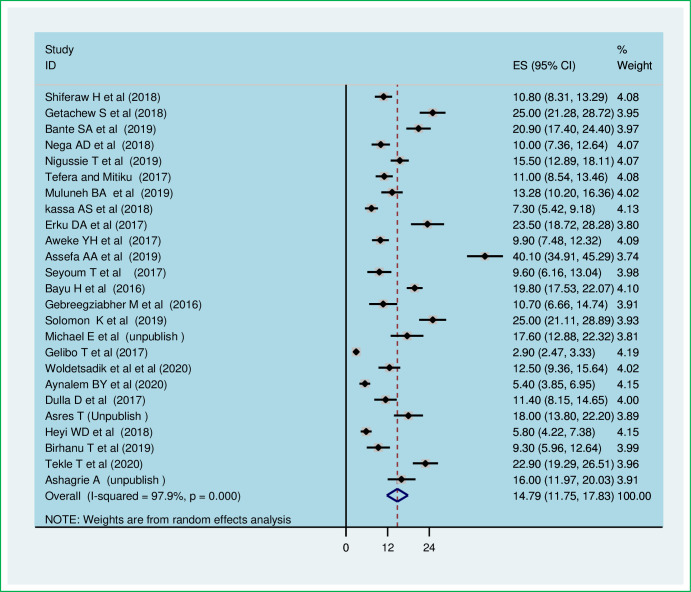
Fig 3. Funnel plot of the prevalence of cervical cancer screening utilization in Ethiopia.
Subgroup analysis
The subgroup analysis was conducted based on region of studies, the study design and women’s characteristics. Therefore, this random effect meta-analysis based on the geographic region revealed that the highest cervical cancer screening utilization was observed in the SNNPR, 18.59 (95% CI: 9.65, 27.53) followed by Oromia region, 16.00% (95% CI: 16.00% (95% CI: 6.31, 25.7) and lowest occurred in Amhara region, 13.62% (95% CI: 9.92, 17.32) ( Table 2 ). In addition, the pooled subgroup analysis showed that cervical cancer screening was highest in studies that were institution- based cross-sectional studies, 17.54% (95% CI: 13.16, 21.93). The highest cervical cancer screening was among HIV- positive women, 20.71% (95% CI: 12.8, 28.63) and the lowest was among reproductive age women, 11.54% (95% CI: 8.00, 15.05) ( Table 2 ).
Table 2. Sub-group analysis of cervical cancer screening utilization in Ethiopia: A meta-analysis.
Predictors of cervical cancer screening utilization, association of educational status and utilization of cervical cancer screening.
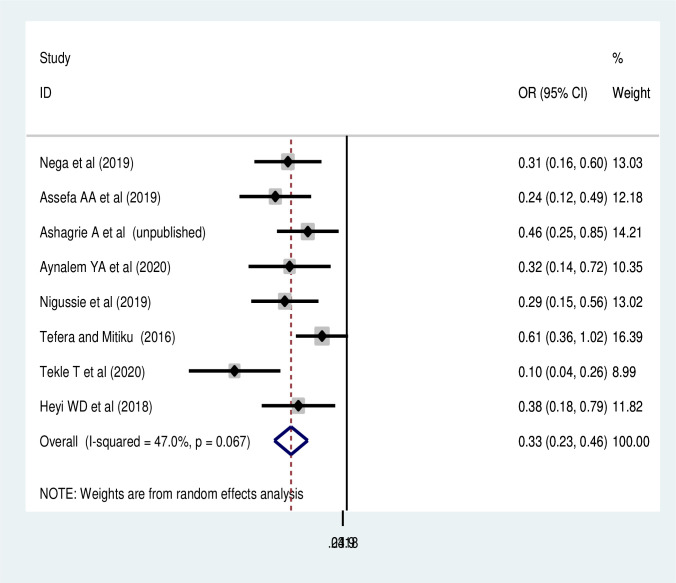
In regard to the social inequities, the effects of three predictors on cervical cancer screening utilization were estimated. Thus, age of women and occupational status were not significantly associated with cervical cancer screening utilization ( S2 and S3 Figs). While, women’s educational status was significantly associated with utilization of cervical cancer screening. Accordingly, the pooled random effect of eight studies [ 48 – 50 , 54 , 57 , 62 , 63 , 60 ] found that women who have no formal education were 66% (POR:0.33, 95% CI: 0.23,0.46) times less likely to utilize cervical cancer screening than those who attended any formal education ( Fig 4 ).
Fig 4. Association of educational status with cervical cancer screening in Ethiopia.
Association of knowledge and perception of cancer and screening utilization
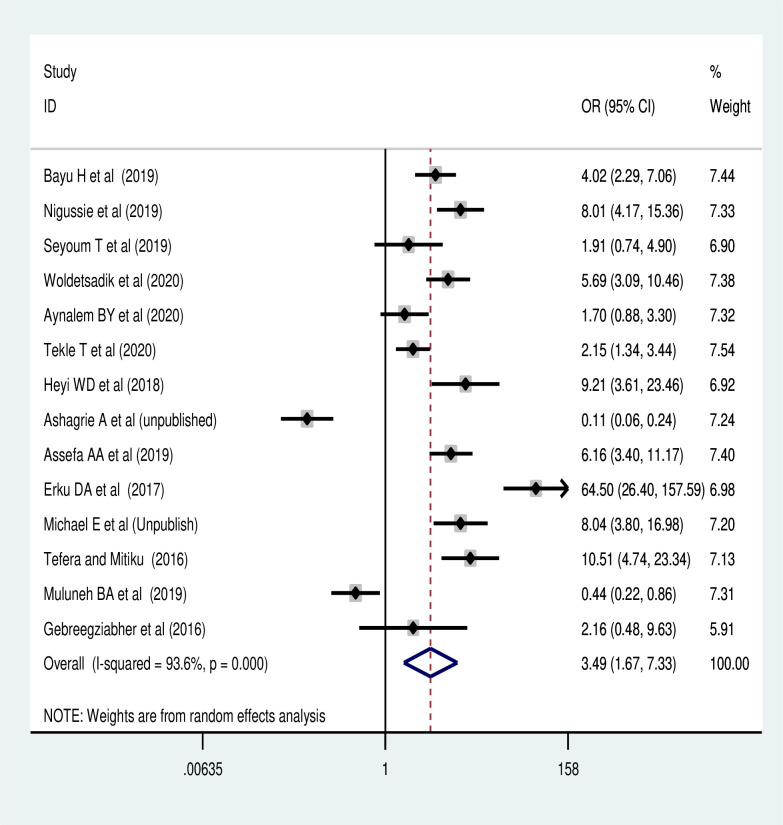
The meta-analysis of 14 studies revealed [ 42 , 45 , 49 – 51 , 53 , 54 , 57 , 58 , 60 , 62 – 65 ] that women’s knowledge of cervical cancer screening uptake was the commonest predictor of screening utilization. Women who had good knowledge of cervical cancer screening reuptake were 3.97 times (POR: 3.49, 95% CI: 1.67, 7.33) more likely to have cervical cancer screening than women who had poor knowledge ( Fig 5 ).
Fig 5. Association of knowledge of the screening with cervical cancer screening utilization.
The pooled effect of six studies [ 33 , 42 , 45 , 49 , 53 , 64 ] also revealed that the perceived susceptibility to cervical cancer was another major predictor of cervical cancer screening utilization in Ethiopia. Women who had perceived susceptibility to cervical cancer were 5.5 times more likely to reuptake cervical cancer screening than their counterparts (POR = 5.54, 95% CI: 4.28, 7.16) ( Fig 6 ). Similarly, women who had perceived severity of cervical cancer were more likely to utilize cervical cancer screening (POR = 6.57, 95% CI: 3.99, 10.82) ( Fig 7 ).
Fig 6. Association of perceived susceptibility to cervical cancer with cervical cancer screening.
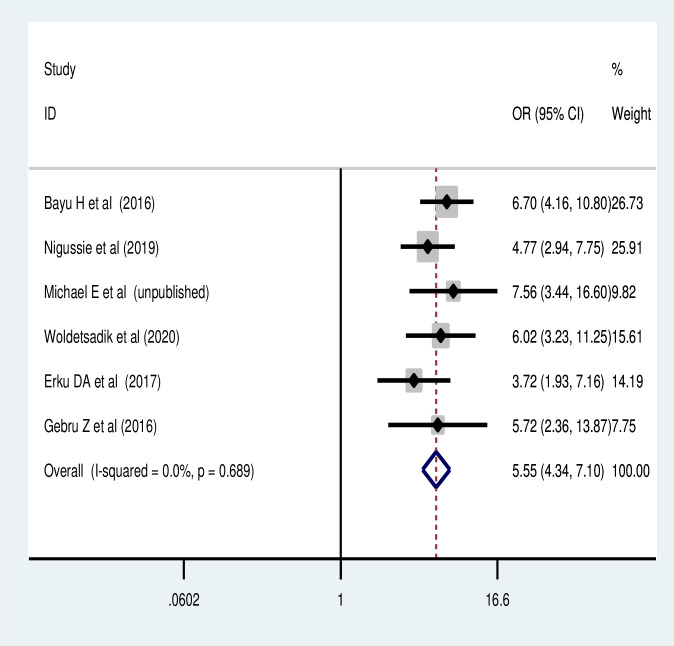
Fig 7. Association of perceived severity of cancer and cervical cancer screening utilization.
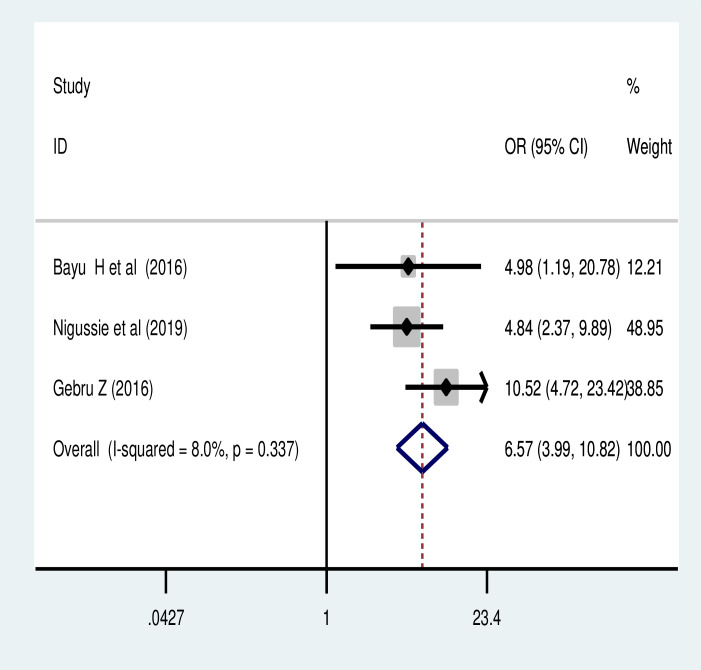
Association of history of sexual transmitted infection and cervical cancer screening uptake
Based on the pooled analysis of four studies [ 47 , 51 , 54 , 64 ], women who had history of sexual transmitted infection were more likely to utilize cervical cancer screening (POR: 3.32, 95% CI: 1.07, 10.34) ( Fig 8 ).
Fig 8. Association of history of sexual transmitted infection with cervical cancer screening utilization.
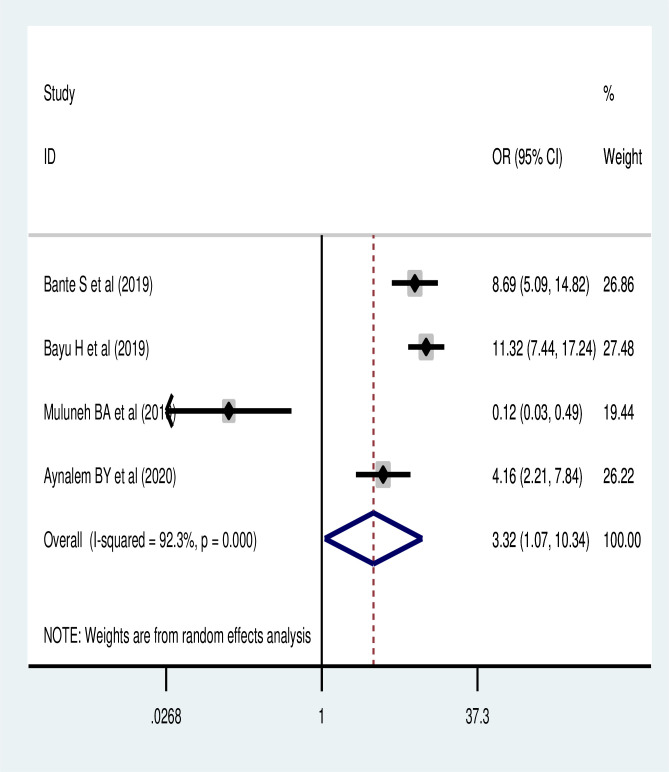
Barriers of cervical cancer screening uptake
The pooled analysis also revealed that the most common reasons that hinder the use of cervical cancer screening were associated with women considered to be healthy, 48.97% (95% CI: 38.3, 59.59) and lack of information on screening, 34.34% (95% CI: (17.93, 50.75) ( Table 3 ).
Table 3. Barriers of the cervical cancer screening utilization in Ethiopia: A meta-analysis.
Discussions.
The uptake of cervical cancer screening services in Ethiopia is not well established. Despite, WHO recommends cervical cancer screening tests to be included as part of well-planned and implemented programs in every country’s health care policy. This systematic review and meta-analysis was conducted to estimate the pooled level of cervical cancer screening and its associated factors in Ethiopia. Accordingly, the pooled national level of cervical cancer screening utilization was 14.79 (95% CI: 11.75, 17.83). This was lower than 85% from a study conducted in United States [ 13 ], 21.4% in China national population based survey [ 67 ], 19.4% in Kenya [ 68 ], 19% - 63% from studies conducted in 54 countries [ 69 ], 48.9% in Malaysia [ 70 ], and also lower than 67% from a national-based study conducted among Vietnamese women [ 71 ]. The difference could be explained by the variation in the population characteristics, study settings and quality of health care services and screening programs. Besides, this could be explained by socio-economic inequalities, higher birth order and poor access to reproductive health care service utilization in Ethiopia could lower the cervical screening utilization. Previous report also showed that women with high birth order and poor women are less likely to receive cervical screening service [ 69 ]. In Ethiopia, a small proportion of women are in contact with obstetric or gynecological health services and that the health system may not have the capacity to provide effective screening to a larger number of women. Therefore, intervention programs to improve the quality of cervical cancer screening clinics are essential.
The findings of this meta-analysis also showed that the highest prevalence of cervical cancer screening occurred in the SNNPR followed by Oromia region and the lowest was in Amhara region. Regional variation in the burden of cervical cancer screening in Ethiopia might be explained by the difference in maternal health care service utilization that could be explained by in the difference in spousal support, cultural and linguistic diversity across the regions and societal stigmatization. Additionally, health service-related reason like cost of access to services, proximity to facilities, navigation of the facilities, waiting time and attitude of the health care staff may be the reasons for the regional difference and lower use of cervical cancer screening in the country.
The highest screening utilization in SNNPR and Oromia may be due to the nature of included studies in the respective regions. For example, 60% of the studies from SNNP region were institutional based cross-sectional studies and 50% of the included studies from Oromia region were conducted among HIV-positive women. Such differences may have contributed to the higher prevalence of cervical cancer screening in SNNPR and Oromia regions. Furthermore, socio-demographic characteristics and lifestyle activities could also be mentioned as reasons for the variation in screening across the different regions in the country. The pooled cervical cancer screening was also highest among HIV- positive women (20.71%). This may be due to the fact that these women may be given information about the disease during their follow-up visit to antiretroviral therapy [ 57 ], which may improve their knowledge about cervical cancer, and therefore, increase service utilization.
This systematic review and meta-analysis found that educational status of women was one of the significant predictors of cervical cancer screening utilization. No formal education reduces the cervical cancer screening uptake by 67%, and this finding was supported by a study done in China [ 67 ] and a meta-analysis conducted in developed countries [ 72 ]. The possible justification for this might be due to the fact that women who have no formal education are less likely to have gynecological examinations and maternal health service utilization. As the result, they are likely to have limited exposure to visit health institution for antenatal care, health facility delivery and post-natal care.
Uneducated women also have lower possibilities to read and fully understand the information and instructions provided by healthcare providers, and therefore, reduce the rate of cervical cancer screening. Cervical cancer educational interventions and provider recommendation for screening increases the rates of cervical cancer screening [ 73 ]. Therefore, more integrated interventions to improve women’s empowerment should be done at national level to improve the rate of cervical cancer screening utilization, and therefore, reduce cervical cancer related morbidity and mortality.
This study also found that women’s knowledge of screening for cervical cancer was a significant predictor of cervical cancer screening service uptake. The finding was supported by studies done in Uganda [ 74 ], Malaysia [ 70 ], a review done in LMICs [ 75 ] and among Arab women [ 76 ]. This could be explained by the fact that those women who had good knowledge for cervical cancer screening are more likely to give priority to the issue and improves their decisions on health- seeking screening behavior. Accordingly, findings in Ethiopia, Malawi, Tanzania and Thailand [ 64 , 77 – 79 ] have shown that a good flow of information and awareness creation campaigns about cervical cancer increase the uptake of cervical cancer screening.
This meta-analysis also showed that women with a history of STI were more likely to use screening for cervical cancer compared to those with no history of STI. This result was supported by the findings of other studies [ 64 , 80 ]. This may be explained by the fact that women who have STIs and history of STI will have an increased chance of visiting health institutions for treatment and medical check-ups, and therefore, more likely to get the screening information from the healthcare provider.
This systematic review and meta-analysis also found that perceived susceptibility and severity were also predictors of the use of cervical cancer screening as supported by Wanyenze et al. [ 74 ]. This may be those who perceive their susceptibility or severity of cancer may be aware of the severity of the cancer and higher level of education about the disease as a result of the increased screening rate. As a result, those women who have an increased perception of susceptibility or severity of the disease may have higher education that has increased adherence to the cervical cancer screening [ 68 ]. These may include those women who are perceived to be more acutely aware of their risk, more interested and knowledgeable about health and behavioral issues, and better access to health information and resources [ 81 ]. This finding was also supported by recent studies done in Ghana [ 82 ] and Kenya [ 83 ] which found that women who perceived the severity of disease were more likely to accept screening due to increased perception of the benefits and barriers to cervical cancer, which increases their cancer screening.
Furthermore, the results of this systematic review and meta-analysis found that the common barriers to the utilization of cervical cancer screening were considered healthy and lack of information by women. This is supported by additional studies [ 47 , 49 , 51 , 56 , 64 ]. This may be due to the fact that those who consider their status to be healthy and who have poor knowledge are less likely to perceive the benefits of screening and the severity of cervical cancer., Therefore, multi-disciplinary interventions across the life course, community education and social mobilization on cervical cancer risk and its screening should be improved and emphasized to increase the cervical cancer screening utilization.
This review’s strengths include the very extensive systematic search conducted and the inclusion of articles identified without specifying the population characteristics and period of publications. Our review adopted the international standard definitions to measure the quality of studies. This meta-analysis has its strengths because it has used a pre-specified protocol for search strategy and data abstraction and used internationally accepted tools for a critical appraisal system for the quality assessment of individual studies.
However, the results of this review should be interpreted with some limitation. The high heterogeneity in the characteristics of the studies might lead to insufficient statistical power to detect significant association. However, a meta-regression analysis revealed that there was no variation due to sample size and publication year. This meta-analysis was also unable to assess the type of screening, and therefore, an area of research for future studies. Additionally, the studies included in this review were from only five regions out of the nine regional states and the two administrative cities that might reduce its representativeness for the country. Some studies have small sample size, affect the estimation.
This meta-analysis found that cervical cancer screening rate was lower than the WHO recommendations. Only one in every seven eligible women were screened in Ethiopia, and there was a significant variation in the screening level based on geographical regions and characteristics of women. Women’s educational status, knowledge towards cervical cancer screening, perceived susceptibility and severity to cervical cancer and history of sexual transmitted infections significantly increased uptake of the screening practice. Therefore, women empowerment, improving knowledge towards cervical cancer screening, enhancing perceived susceptibility and severity to cervical cancer and identifying previous history of women are an essential strategy to increase utilization of cancer screening. Moreover, adoption of the better strategies and addressing the barriers of cervical cancer screening uptake mainly improving of the provision of adequate information on cervical cancer screening has a paramount importance to improve cervical cancer screening among reproductive age women.
Supporting information
Abbreviations.
Community Based Cross-sectional Studies
Facility- Based Cross-sectional Studies
Human Immunodeficiency Virus
Human Papilloma Virus
Low and Middle-Income Countries
Pooled Odds Ratio
Southern Nations, Nationalities and Peoples Representative
Sub Saharan Africa
Sexually Transmitted Infection, WHO: World Health Organization
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
- 1. WHO U, PATH. cryosurgical equipment for the treatment of precancerous cervical lesions and prevention of cervical cancer. 2012.
- 2. WHO/NMH/NMA. UN Joint Global Programme on Cervical Cancer Prevention and Control. The United Nations Global Cervical Cancer Programme 2016.
- 3. Bruni L, Albero G, Serrano B, Mena M, Gómez D, Muñoz J, et al. Human Papillomavirus and Related Diseases in Ethiopia. 2017. [ Google Scholar ]
- 4. Fitzmaurice C, Dicker D, Pain A, Hamavid H, Moradi-Lakeh M, MacIntyre MF, et al. The Global Burden of Cancer 2013. JAMA oncology. 2015;1(4):505–27. Epub 2015/07/17. doi: 10.1001/jamaoncol.2015.0735 ; PubMed Central PMCID: PMC4500822. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. Hendry M, Lewis R, Clements A, Damery S, Clare W. "HPV? Never heard of it!": A systematic review of girls’ and parents’ information needs, views and preferences about human papillomavirus vaccination 2013. doi: 10.1016/j.vaccine.2013.08.091 [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Health WHOR, Diseases WHOC, Promotion H. Comprehensive cervical cancer control: a guide to essential practice: World Health Organization; 2006. [ PubMed ]
- 7. Denny L, Quinn M, Sankaranarayanan R. Screening for cervical cancer in developing countries. Vaccine. 2006;24:S71–S7. doi: 10.1016/j.vaccine.2006.05.121 [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. Sankaranarayanan R et al. HPV screening for cervical cancer in rural India. N Engl J Med. 2009;360: 1385–1394. doi: 10.1056/NEJMoa0808516 [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Moyer VA. Screening for cervical cancer: US Preventive Services Task Force recommendation statement. Annals of internal medicine. 2012;156(12):880–91. doi: 10.7326/0003-4819-156-12-201206190-00424 [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. FMOH. National cancer control plan of Ethiopia. 2015.
- 11. Campos NG, Castle PE, Wright TC Jr, Kim JJ. Cervical cancer screening in low‐resource settings: A cost‐effectiveness framework for valuing tradeoffs between test performance and program coverage. International journal of cancer. 2015;137(9):2208–19. doi: 10.1002/ijc.29594 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 12. Pimple S, Mishra G, Shastri S. Global strategies for cervical cancer prevention. Current Opinion in Obstetrics and Gynecology. 2016;28(1):4–10. doi: 10.1097/GCO.0000000000000241 [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. (OECD. StatExtracts; 2013. http://stats.oecd.org/Index.aspx?DataSetCode=HEALTH_PROC . Cited May 6 2020.).
- 14. Sudenga SL, Rositch AF, Otieno WA, Smith JS. Knowledge, attitudes, practices, and perceived risk of cervical cancer among Kenyan women: brief report. International Journal of Gynecologic Cancer. 2013;23(5):895–9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 15. Idowu A, Olowookere SA, Fagbemi AT, Ogunlaja OA. Determinants of cervical cancer screening uptake among women in Ilorin, North Central Nigeria: a community-based study. Journal of cancer epidemiology. 2016;2016. doi: 10.1155/2016/6469240 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 16. Ngugi CW BH, Muigai AW, Wanzala P, Mbithi JN. Factors affecting uptake of cervical cancer early detection measures among women in Thika, Kenya. Health Care Women Int. 2012;33(595–613 doi: 10.1080/07399332.2011.646367 ]. [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. De Sanjosé S, Serrano B, Castellsagué X, Brotons M, Muñoz J, Bruni L, et al. Human papillomavirus (HPV) and related cancers in the Global Alliance for Vaccines and Immunization (GAVI) countries. A WHO/ICO HPV Information Centre Report. Vaccine. 2012;30(Suppl 4):D1–83. [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Chidyaonga-Maseko F, Chirwa ML, Muula AS. Underutilization of cervical cancer prevention services in low and middle income countries: a review of contributing factors. Pan African medical journal. 2015;21(1). doi: 10.11604/pamj.2015.21.231.6350 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. Moher D et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic reviews. 2015;4(1). doi: 10.1186/2046-4053-4-1 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 20. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). Jama. 2016;315(8):801–10. doi: 10.1001/jama.2016.0287 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 21. Egger M SG, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. doi: 10.1136/bmj.315.7109.629 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 22. Begg CB MM. Operating characteristics of a rank correlation testfor publication bias. Biometrics. 1994;50(4):1088–101. [ PubMed ] [ Google Scholar ]
- 23. Higgins JP TS, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557. doi: 10.1136/bmj.327.7414.557 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 24. Deeks JJ, Higgins JP, Altman DG. Analysing data and undertaking meta‐analyses. Cochrane handbook for systematic reviews of interventions. 2008:241–84. [ Google Scholar ]
- 25. Teame H, Gebremariam L, Kahsay T, Berhe K, Gebreheat G. Factors affecting utilization of cervical cancer screening services among women attending public hospitals in Tigray region, Ethiopia, 2018; Case control study. 2019;14(3):e0213546. doi: 10.1371/journal.pone.0213546 . [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 26. Geremew AB, Gelagay AA, Azale T. Comprehensive knowledge on cervical cancer, attitude towards its screening and associated factors among women aged 30–49 years in Finote Selam town, northwest Ethiopia. Reproductive health. 2018;15(1):29. Epub 2018/02/16. doi: 10.1186/s12978-018-0471-1 ; PubMed Central PMCID: PMC5813403. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 27. Petros H, Ayele AA. Cervical Cancer Screening and Treatment Services in South West Shoa Zone of Oromia Region. Ethiopian Journal of Reproductive Health. 2018;10(1):7–. [ Google Scholar ]
- 28. Gebrie MH, Belete MA, Lemlem SB, Woreta HK. Knowledge, preventive practice and associated factors of female nurses’ towards cervical cancer in the selected government hospitals in Addis Ababa, Ethiopia. J Diabetes Metab. 2015;6(7):569. [ Google Scholar ]
- 29. Tarekegn AA, Mengistu MY, Mirach TH. Health professionals’ willingness to pay and associated factors for cervical cancer screening program at College of Medicine and Health Sciences, University of Gondar, Northwest Ethiopia. PloS one. 2019;14(4). doi: 10.1371/journal.pone.0215904 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 30. Bejiga B. Acceptability of cervical cancer screening using See and Treat (SAT) approachand determinant factors among women of reproductive age in health centers in Addis Ababa, Ethiopia 2017. [ Google Scholar ]
- 31. Boka A, Nigatu D. Cervical cancer screening and associated factors among women attending gynecology out-patient department and maternal and child health atmettu karlreferralhospital, South West, Ethiopia, 2019. International Journal of Current Research in Life Sciences. 8(01):2934–44. [ Google Scholar ]
- 32. Deribe L. cervical cancer screening service utilization and associated factors among HIV positive and women with unknown hiv status in alamata generalized hospital, Tigray, Ethiopia 2018: comparative cross sectional study: Addis Ababa Universty; 2018. [ Google Scholar ]
- 33. Gebru Z, Gerbaba M, Dirar A. Utilization of Cervical Carcinoma Screening Service and Associated Factors among Currently Married Women in Arba Minch Town, Southern Ethiopia Journal of Womens Health Care. 2016;5(1). [ Google Scholar ]
- 34. Tilahun T, Tulu T, Dechasa W. Knowledge, attitude and practice of cervical cancer screening and associated factors amongst female students at Wollega University, western Ethiopia. BMC research notes. 2019;12(1):518. doi: 10.1186/s13104-019-4564-x [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 35. Mulatu K, Motma A, Seid M, Tadesse M. Assessment of knowledge, attitude and practice on cervical cancer screening among female students of Mizan Tepi University, Ethiopia, 2016. Cancer Biol Ther Oncol. 2017;1(1):1–5. [ Google Scholar ]
- 36. Mekuria R. cervical cancer screening behavior and associated factors among women attending gynecology out-patient department and maternal and child health Atdilla university referral hospital, Ethiopia, 2018: Addis Ababa University; 2018. [ Google Scholar ]
- 37. Tsegaye S. Knowledge, Attitude, Practice of Cervical Cancer Screening and Its Associated Factors Among Female Students in Hawassa Universitycollege of Medicine and Health Science Hawassa: Addis Ababa University; 2015. [ Google Scholar ]
- 38. Abdulkadir IR. Level of knowledge toward human papillomavirus/cervical cancer & practice of Papanicolaou test screening among female Addis Ababa university students in Ethiopia: California State University, Northridge; 2013. [ Google Scholar ]
- 39. Gebregziabher D, Berhanie E, Birhanu T, Tesfamariam K. Correlates of cervical cancer screening uptake among female under graduate students of Aksum University, College of Health Sciences, Tigray, Ethiopia. BMC research notes. 2019;12(1):520. Epub 2019/08/21. doi: 10.1186/s13104-019-4570-z ; PubMed Central PMCID: PMC6701026. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 40. Mersha A. Comprehensive knowledge and uptake of cervical cancer screening is low among women living with HIV/AIDS in Northwest Ethiopia. Value in Health. 2017;20(9):A493. doi: 10.1186/s40661-017-0057-6 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 41. Gelibo T, Roets L, Getachew T, Bekele A. Coverage and factors associated with cervical Cancer screening: results from a population-based WHO steps Study in Ethiopia. Adv Oncol Res Treat. 2017;1(115):2. [ Google Scholar ]
- 42. Michael E. Cervical cancer screening utilization and its associated factors among women aged 30 years and above in Woliso town, South West Showa Zone, Oromia region, Ethiopia: Addis Ababa Universty; 2018. [ Google Scholar ]
- 43. Shiferaw S, Addissie A. Knowledge about cervical cancer and barriers toward cervical cancer screening among HIV-positive women attending public health centers in Addis Ababa city, Ethiopia. 2018;7(3):903–12. doi: 10.1002/cam4.1334 . [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 44. Getachew S, Getachew E. Cervical cancer screening knowledge and barriers among women in Addis Ababa, Ethiopia. 2019;14(5):e0216522. doi: 10.1371/journal.pone.0216522 . [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 45. Woldetsadik AB, Amhare AF, Bitew ST, Pei L, Lei J, Han J. Socio-demographic characteristics and associated factors influencing cervical cancer screening among women attending in St. Paul’s Teaching and Referral Hospital, Ethiopia. BMC women’s health. 2020;20(1):70. Epub 2020/04/08. doi: 10.1186/s12905-020-00927-5 ; PubMed Central PMCID: PMC7137499. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 46. Birhanu Z, Abdissa A, Belachew T, Deribew A, Segni H, Tsu V, et al. Health seeking behavior for cervical cancer in Ethiopia: a qualitative study. International journal for equity in health. 2012;11:83. Epub 2013/01/01. doi: 10.1186/1475-9276-11-83 ; PubMed Central PMCID: PMC3544623. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 47. Bante SA, Getie SA, Getu AA, Mulatu K, Fenta SL. Uptake of pre-cervical cancer screening and associated factors among reproductive age women in Debre Markos town, Northwest Ethiopia, 2017. BMC public health. 2019;19(1):1102. Epub 2019/08/16. doi: 10.1186/s12889-019-7398-5 ; PubMed Central PMCID: PMC6692942. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 48. Nega AD, Woldetsadik MA, Gelagay AA. Low uptake of cervical cancer screening among HIV positive women in Gondar University referral hospital, Northwest Ethiopia: cross-sectional study design. 2018;18(1):87. Epub 2018/07/10. doi: 10.1186/s12905-018-0579-z . [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 49. Nigussie T, Admassu B, Nigussie A. Cervical cancer screening service utilization and associated factors among age-eligible women in Jimma town using health belief model, South West Ethiopia. BMC women’s health. 2019;19(1):127. Epub 2019/10/30. doi: 10.1186/s12905-019-0826-y ; PubMed Central PMCID: PMC6819648. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 50. Tefera F, Mitiku I. Uptake of Cervical Cancer Screening and Associated Factors Among 15-49-Year-Old Women in Dessie Town, Northeast Ethiopia. Journal of cancer education: the official journal of the American Association for Cancer Education. 2017;32(4):901–7. Epub 2016/04/15. doi: 10.1007/s13187-016-1021-6 . [ DOI ] [ PubMed ] [ Google Scholar ]
- 51. Muluneh BA, Atnafu DD, Wassie B. Predictors of cervical cancer screening service utilization among commercial sex workers in Northwest Ethiopia: a case-control study. BMC women’s health. 2019;19(1):162. doi: 10.1186/s12905-019-0862-7 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 52. Kasa AS, Tesfaye TD, Temesgen WA. Knowledge, attitude and practice towards cervical cancer among women in Finote Selam city administration, West Gojjam Zone, Amhara Region, North West Ethiopia, 2017. African health sciences. 2018;18(3):623–36. doi: 10.4314/ahs.v18i3.20 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 53. Erku DA, Netere AK, Mersha AG, Abebe SA, Mekuria AB, Belachew SA. Comprehensive knowledge and uptake of cervical cancer screening is low among women living with HIV/AIDS in Northwest Ethiopia. Gynecologic oncology research and practice. 2017;4(1):20. doi: 10.1186/s40661-017-0057-6 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 54. Aynalem BY, Anteneh KT, Enyew MM. Utilization of cervical cancer screening and associated factors among women in Debremarkos town, Amhara region, Northwest Ethiopia: Community based cross-sectional study. PloS one. 2020;15(4):e0231307. Epub 2020/04/08. doi: 10.1371/journal.pone.0231307 ; PubMed Central PMCID: PMC7138328. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 55. ASERES T. KNOWLEDGE, PRACTICE AND ASSOCIATED FACTORS OF CERVICAL CANCER SCREENING AMONG WOMEN HEALTH WORKERS IN GONDAR UNIVERSITY TEACHING AND REFERRAL HOSPITAL, GONDAR, ETHIOPIA, 2016 2017.
- 56. Aweke YH, Ayanto SY, Ersado TL. Knowledge, attitude and practice for cervical cancer prevention and control among women of childbearing age in Hossana Town, Hadiya zone, Southern Ethiopia: Community-based cross-sectional study. PloS one. 2017;12(7):e0181415. Epub 2017/07/26. doi: 10.1371/journal.pone.0181415 ; PubMed Central PMCID: PMC5526548. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 57. Assefa AA, Astawesegn FH, Eshetu B. Cervical cancer screening service utilization and associated factors among HIV positive women attending adult ART clinic in public health facilities, Hawassa town, Ethiopia: a cross-sectional study. BMC health services research. 2019;19(1):847. Epub 2019/11/21. doi: 10.1186/s12913-019-4718-5 . [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 58. Seyoum T, Yesuf A, Kejela G, Gebremeskel F. Utilization of cervical cancer screening and associated factors among female health Workers in Governmental Health Institution of Arba Minch town and Zuria District, Gamo Gofa zone, Arba Minch, Ethiopia, 2016. Arch Cancer Res. 2017;5(4):165. [ Google Scholar ]
- 59. Dulla D, Daka D, Wakgari N. Knowledge about cervical cancer screening and its practice among female health care workers in southern Ethiopia: a cross-sectional study. International journal of women’s health. 2017;9:365. doi: 10.2147/IJWH.S132202 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 60. Tekle T, Wolka E, Nega B, Kumma WP, Koyira MM. Knowledge, Attitude and Practice Towards Cervical Cancer Screening Among Women and Associated Factors in Hospitals of Wolaita Zone, Southern Ethiopia. Cancer management and research. 2020;12:993. doi: 10.2147/CMAR.S240364 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 61. Solomon K, Tamire M, Kaba M. Predictors of cervical cancer screening practice among HIV positive women attending adult anti-retroviral treatment clinics in Bishoftu town, Ethiopia: the application of a health belief model. BMC cancer. 2019;19(1):989. Epub 2019/10/28. doi: 10.1186/s12885-019-6171-6 ; PubMed Central PMCID: PMC6813043. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 62. Heyi WD, Bekabil TT, Ebo GG. KNOWLEDGE, ATTITUDE AND PRACTICE OF CERVICAL CANCER SCREENING AMONG WOMEN AGED 15–49 YEARS IN BISHOFTU TOWN, EAST SHEWA ZONE, OROMIA REGION, ETHIOPIA, 2016. Ethiopian Journal of Reproductive Health. 2018;10(2):10–. [ Google Scholar ]
- 63. Ashagrie A. Knowledge and screening practice on cervical cancer and associated factors among HIV positive women in Adama, Ethiopia: Addis Ababa Universty; 2017. doi: 10.1186/s13104-017-2887-z [ DOI ] [ Google Scholar ]
- 64. Bayu H, Berhe Y, Mulat A, Alemu A. Cervical Cancer Screening Service Uptake and Associated Factors among Age Eligible Women in Mekelle Zone, Northern Ethiopia, 2015: A Community Based Study Using Health Belief Model. PloS one. 2016;11(3):e0149908. Epub 2016/03/11. doi: 10.1371/journal.pone.0149908 ; PubMed Central PMCID: PMC4786115. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 65. Gebreegziabher M, Asefa NG, Berhe S. Factors Affecting the Practices of Cervical Cancer Screening among Female Nurses at Public Health Institutions in Mekelle Town, Northern Ethiopia, 2014: A Cross-Sectional Study. Journal of Cancer Research. 2016;2016. [ Google Scholar ]
- 66. Berhanu T, Mamo E, Tewolde T, Beshir M. Knowledge of Cervical Cancer and Its Screening Practice among Health Extension Workers in Addis Ababa, Ethiopia. Primary Health Care: Open Access. 2019;9(1):1–5. [ Google Scholar ]
- 67. Bao H, Zhang L, Wang L, Zhang M, Zhao Z, Fang L, et al. Significant variations in the cervical cancer screening rate in China by individual‐level and geographical measures of socioeconomic status: a multilevel model analysis of a nationally representative survey dataset. Cancer medicine. 2018;7(5):2089–100. doi: 10.1002/cam4.1321 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 68. Tiruneh FN, Chuang K-Y, Ntenda PAM, Chuang Y-C. Individual-level and community-level determinants of cervical cancer screening among Kenyan women: a multilevel analysis of a Nationwide survey. BMC women’s health. 2017;17(1):109. doi: 10.1186/s12905-017-0469-9 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 69. Gakidou E, Nordhagen S, Obermeyer Z. Coverage of cervical cancer screening in 57 countries: low average levels and large inequalities. PLoS medicine. 2008;5(6). doi: 10.1371/journal.pmed.0050132 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 70. Gan DEH, Dahlui M. Cervical screening uptake and its predictors among rural women in Malaysia. Singapore medical journal. 2013;54(3):163–8. doi: 10.11622/smedj.2013047 [ DOI ] [ PubMed ] [ Google Scholar ]
- 71. Ho V, Yamal JM, Atkinson EN, Basen-Engquist K, Tortolero-Luna G, Follen M. Predictors of Breast and Cervical Screening in Vietnamese Women in Harris County, Houston, Texas. Cancer Nursing. 2005;28(2):119–29. 00002820-200503000-00005. doi: 10.1097/00002820-200503000-00005 [ DOI ] [ PubMed ] [ Google Scholar ]
- 72. Damiani G, Basso D, Acampora A, Bianchi CB, Silvestrini G, Frisicale EM, et al. The impact of level of education on adherence to breast and cervical cancer screening: evidence from a systematic review and meta-analysis. Preventive medicine. 2015;81:281–9. doi: 10.1016/j.ypmed.2015.09.011 [ DOI ] [ PubMed ] [ Google Scholar ]
- 73. Musa J, Achenbach CJ, O’Dwyer LC, Evans CT, McHugh M, Hou L, et al. Effect of cervical cancer education and provider recommendation for screening on screening rates: A systematic review and meta-analysis. PloS one. 2017;12(9). doi: 10.1371/journal.pone.0183924 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 74. Wanyenze RK, Bwanika JB, Beyeza-Kashesya J, Mugerwa S, Arinaitwe J, Matovu JK, et al. Uptake and correlates of cervical cancer screening among HIV-infected women attending HIV care in Uganda. Global health action. 2017;10(1):1380361. doi: 10.1080/16549716.2017.1380361 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 75. Devarapalli P, Labani S, Nagarjuna N, Panchal P, Asthana S. Barriers affecting uptake of cervical cancer screening in low and middle income countries: A systematic review. Indian journal of cancer. 2018;55(4):318. doi: 10.4103/ijc.IJC_253_18 [ DOI ] [ PubMed ] [ Google Scholar ]
- 76. Abboud S, De Penning E, Brawner BM, Menon U, Glanz K, Sommers MS, editors. Cervical cancer screening among Arab women in the United States: an integrative review. Oncology nursing forum; 2017: NIH Public Access. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 77. Lyimo FS, Beran TN. Demographic, knowledge, attitudinal, and accessibility factors associated with uptake of cervical cancer screening among women in a rural district of Tanzania: three public policy implications. BMC public health. 2012;12(1):22. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 78. Chosamata MS, Hong SA, Tiraphat S. Determinants of cervical cancer screening utilization among women aged 30–45 years in Blantyre district, Malawi. 2015. [ Google Scholar ]
- 79. Visanuyothin S, Chompikul J, Mongkolchati A. Determinants of cervical cancer screening adherence in urban areas of Nakhon Ratchasima Province, Thailand. Journal of infection and public health. 2015;8(6):543–52. doi: 10.1016/j.jiph.2015.04.018 . [ DOI ] [ PubMed ] [ Google Scholar ]
- 80. Teame H, Addissie A, Ayele W, Hirpa S, Gebremariam A, Gebreheat G, et al. Factors associated with cervical precancerous lesions among women screened for cervical cancer in Addis Ababa, Ethiopia: A case control study. PLOS ONE. 2018;13(1):e0191506. doi: 10.1371/journal.pone.0191506 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 81. Ross CE, Wu C-l. The links between education and health. American sociological review. 1995:719–45.
- 82. Ebu NI, Ogah JK. Predictors of cervical cancer screening intention of HIV-positive women in the central region of Ghana. BMC women’s health. 2018;18(1):43. doi: 10.1186/s12905-018-0534-z [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 83. KAMBAGA EM. Determinants of provider-initiated HIV testing and counselling uptake in Jaramogi Oginga Odinga teaching and referral hospital, Kisumu, Kenya: Maseno University; 2017. [ Google Scholar ]
Decision Letter 0
Nicola Stead
16 Dec 2020
PONE-D-20-22948
Cervical cancer screening utilization and predictors among reproductive-age women in Ethiopia: a systematic review and meta-analysis
Dear Dr. Desta,
Thank you for submitting your manuscript to PLOS ONE. After careful consideration, we feel that it has merit but does not fully meet PLOS ONE’s publication criteria as it currently stands. Therefore, we invite you to submit a revised version of the manuscript that addresses the points raised during the review process.
Two reviewers have evaluated your manuscript and are largely positive about the study. However, they have asked for further details regarding the the choice of age range as well as outlining the limitations of the study and it's generalizability for the study areas.
Please submit your revised manuscript by Jan 29 2021 11:59PM. If you will need more time than this to complete your revisions, please reply to this message or contact the journal office at [email protected] . When you're ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
Please include the following items when submitting your revised manuscript:
A rebuttal letter that responds to each point raised by the academic editor and reviewer(s). You should upload this letter as a separate file labeled 'Response to Reviewers'.
A marked-up copy of your manuscript that highlights changes made to the original version. You should upload this as a separate file labeled 'Revised Manuscript with Track Changes'.
An unmarked version of your revised paper without tracked changes. You should upload this as a separate file labeled 'Manuscript'.
If you would like to make changes to your financial disclosure, please include your updated statement in your cover letter. Guidelines for resubmitting your figure files are available below the reviewer comments at the end of this letter.
If applicable, we recommend that you deposit your laboratory protocols in protocols.io to enhance the reproducibility of your results. Protocols.io assigns your protocol its own identifier (DOI) so that it can be cited independently in the future. For instructions see: http://journals.plos.org/plosone/s/submission-guidelines#loc-laboratory-protocols
We look forward to receiving your revised manuscript.
Kind regards,
Senior Editor
Journal Requirements:
When submitting your revision, we need you to address these additional requirements.
1. Please ensure that your manuscript meets PLOS ONE's style requirements, including those for file naming. The PLOS ONE style templates can be found at
https://journals.plos.org/plosone/s/file?id=wjVg/PLOSOne_formatting_sample_main_body.pdf and
https://journals.plos.org/plosone/s/file?id=ba62/PLOSOne_formatting_sample_title_authors_affiliations.pdf
2. We suggest you thoroughly copyedit your manuscript for language usage, spelling, and grammar. If you do not know anyone who can help you do this, you may wish to consider employing a professional scientific editing service.
Whilst you may use any professional scientific editing service of your choice, PLOS has partnered with both American Journal Experts (AJE) and Editage to provide discounted services to PLOS authors. Both organizations have experience helping authors meet PLOS guidelines and can provide language editing, translation, manuscript formatting, and figure formatting to ensure your manuscript meets our submission guidelines. To take advantage of our partnership with AJE, visit the AJE website ( http://learn.aje.com/plos/ ) for a 15% discount off AJE services. To take advantage of our partnership with Editage, visit the Editage website ( www.editage.com ) and enter referral code PLOSEDIT for a 15% discount off Editage services. If the PLOS editorial team finds any language issues in text that either AJE or Editage has edited, the service provider will re-edit the text for free.
Upon resubmission, please provide the following:
The name of the colleague or the details of the professional service that edited your manuscript
A copy of your manuscript showing your changes by either highlighting them or using track changes (uploaded as a *supporting information* file)
A clean copy of the edited manuscript (uploaded as the new *manuscript* file)
3. Your ethics statement should only appear in the Methods section of your manuscript. If your ethics statement is written in any section besides the Methods, please move it to the Methods section and delete it from any other section. Please ensure that your ethics statement is included in your manuscript, as the ethics statement entered into the online submission form will not be published alongside your manuscript.
[Note: HTML markup is below. Please do not edit.]
Reviewers' comments:
Reviewer's Responses to Questions
Comments to the Author
1. Is the manuscript technically sound, and do the data support the conclusions?
The manuscript must describe a technically sound piece of scientific research with data that supports the conclusions. Experiments must have been conducted rigorously, with appropriate controls, replication, and sample sizes. The conclusions must be drawn appropriately based on the data presented.
Reviewer #1: Yes
Reviewer #2: Yes
2. Has the statistical analysis been performed appropriately and rigorously?
3. Have the authors made all data underlying the findings in their manuscript fully available?
The PLOS Data policy requires authors to make all data underlying the findings described in their manuscript fully available without restriction, with rare exception (please refer to the Data Availability Statement in the manuscript PDF file). The data should be provided as part of the manuscript or its supporting information, or deposited to a public repository. For example, in addition to summary statistics, the data points behind means, medians and variance measures should be available. If there are restrictions on publicly sharing data—e.g. participant privacy or use of data from a third party—those must be specified.
4. Is the manuscript presented in an intelligible fashion and written in standard English?
PLOS ONE does not copyedit accepted manuscripts, so the language in submitted articles must be clear, correct, and unambiguous. Any typographical or grammatical errors should be corrected at revision, so please note any specific errors here.
5. Review Comments to the Author
Please use the space provided to explain your answers to the questions above. You may also include additional comments for the author, including concerns about dual publication, research ethics, or publication ethics. (Please upload your review as an attachment if it exceeds 20,000 characters)
Reviewer #1: General comment: Very good and useful review that could provide evidence on barrier to CC screening in Ethiopia
Specific comments
IN the abstract as well as under background section, it is stated “Despite a remarkable progress in the reduction of maternal mortality, cervical cancer is the 73 second most commonly diagnosed cancer and the leading cause of cancer related death among 74 African women”. I agree with the reduction of MM. However, in view of the fact that CC is a major public health challenge and with its continued pressure, is it not naïve to argue about reduction of maternal mortality without showing how CC screening has contributed to that or contrary to this maintained MM in consequence higher.
Mention is made “The incidence, death rate and morbidities associated with cervical cancer is 79 significantly varies across the world; higher in the developing nations than compared to the 80 developed countries”(4), while again it is stated “The prevalence of cervical cancer screening is much higher at the Western countries than SSA” (11, 12); The two statements looks contradictory
There is no clarity on whether this review is ‘systematic’ or ‘met-analysis’ or ‘both’. If it is both, it is imperative to clarify which part of it is systematic and meta-analysis OR clarify why both were considered.
From the statement “All published and unpublished studies through April 7, 2020” there were quite few concerns. Firstly what was the lower time frame. Could it be any document from time immemorial to April 7, 2020? Secondly, how were the unpublished reports captured? Were there any criterion set to identify those?
While WHO’s recommended age of CC screening is 30-50, it is not clear why in this study age 18-49 years was chosen? Is it not contradictory?
The studies were drawn from five geographic regions: Addis Ababa, Amhara, Southern Nations, Nationalities and Peoples, Oromia and Tigray with only one from the national- level study. Couple of concern here. Firstly, how was the 18,067 women considered to estimate the pooled… proportionated in light of population size. Given the fact that studies are not proportional to the population of the regions, it would be difficult to reach conclusion as desired – this is about comparability of results. Secondly, I am wondering if this study could mirror realities for the country at large. Perhaps clarifying those and stating limitations may help.
I am not convinced that what are stated as ‘most common reasons that hinder the use of cervical cancer screening’ in the result section and conclusion section are aligned. This needs to be checked against the finding and corrected
The fact that it was not clear on what of this review is meta and systematic, the discussion suffers much missing what is being discussed. Perhaps with clarification on how the two contributed to this review may
Reviewer #2: Generally a good paper, congratulations, however, the work needs some grammatic revision for clarity. I have listed some below but kindly revise the entire paper checking for grammatic and punctuation errors.
Line 74- Update the reference and use more recent data than 2013
Line 77- Be consistent in presenting figures i.e 311000 should have a comma as with other figures
Line 78- Correct the grammar of the sentence which start as "The incidence, death ......"
Line 85-6- Correct the grammar of the sentence
Line 97-98- Correct grammar
Line 99-100- Correct grammar
Line 103- Correct the punctuation
Line 292-295- Sentence needs revision for clarity, attend to the grammar
Line 295-298- Sentence needs some revision for clarity
Line 307 - Clarify what "tall reproductive age" refers, sentence may need some revisions
Line 309- Add reference of relevant papers to support your interpretation
Line 367- Replace "representative" with representativeness
6. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
If you choose “no”, your identity will remain anonymous but your review may still be made public.
Do you want your identity to be public for this peer review? For information about this choice, including consent withdrawal, please see our Privacy Policy .
Reviewer #1: Yes: Mirgissa Kaba
Reviewer #2: Yes: Dr. Oscar Tapera
[NOTE: If reviewer comments were submitted as an attachment file, they will be attached to this email and accessible via the submission site. Please log into your account, locate the manuscript record, and check for the action link "View Attachments". If this link does not appear, there are no attachment files.]
While revising your submission, please upload your figure files to the Preflight Analysis and Conversion Engine (PACE) digital diagnostic tool, https://pacev2.apexcovantage.com/ . PACE helps ensure that figures meet PLOS requirements. To use PACE, you must first register as a user. Registration is free. Then, login and navigate to the UPLOAD tab, where you will find detailed instructions on how to use the tool. If you encounter any issues or have any questions when using PACE, please email PLOS at [email protected] . Please note that Supporting Information files do not need this step.
Submitted filename: CC meta-systematic analysis-Review comment.docx
Author response to Decision Letter 0
Collection date 2021.
Dear editors and reviewer of Plos One
We would like to extend our deepest appreciation for devoting your time to review our manuscript entitled “cervical cancer screening utilization and predictors among eligible women in Ethiopia: a systematic review and meta- analysis”. Cervical cancer is the second most commonly diagnosed cancer and the leading cause of cancer death in African women. In 2013, there were approximately 236,000 deaths from cervical cancer worldwide and it is the most common cancer in east and middle Africa. Cervical cancer screening is an important intervention to redcue cervical cancer and its associated maternal mortality. Even though, the utilization of the screening is inconsistent across the country and affected by different barrier. Therefore, this systematic review and meta-analysis estimates the pooled utilization of cervical cancer screening and its predictors in Ethiopia. Overall the main finding of this review is means of an intervention based on the pooled cervical cancer screening utilization and its predictors, which might be used to improve maternal adverse outcomes in Low and middle income countries, subsequently means of achieving SDGs.
Dear reviewer, there has been a major revision of the whole structure of the manuscript (Abstract, introduction, methods, results, discussion and conclusions) mainly with a correction of grammar errors. The further details regarding the choice of age range as well as outlining the limitations of the study and it's generalizability for the study areas are addressed. The reproductive group is substituted by eligible women as the global and who recommendations. We hope now the manuscript is clear and more acceptable than its previous version. We tried to state the limitations and generalizability issues in the limitation and strength section of the discussion. We have tried to present the response for each reviewer according to your comment what to suppose to do so. For this, here we have given our responses to each of the concerns you raised, highlighted by red color. Again, we would like to remind our strongest gratitude for your effort for the improvement of this manuscript and the response for each the points were addressed in the response to reviewers’ section. For this, I kindly request you to consider the paper for publication. Again, we would like to remind our strongest gratitude for your effort for the improvement of this manuscript.
Reviewer #1
1. Abstract
1.1. In the abstract as well as under background section, it is stated “Despite a remarkable progress in the reduction of maternal mortality, cervical cancer is the 73 second most commonly diagnosed cancer and the leading cause of cancer related death among 74 African women”. I agree with the reduction of MM. However, in view of the fact that CC is a major public health challenge and with its continued pressure, is it not naïve to argue about reduction of maternal mortality without showing how CC screening has contributed to that or contrary to this maintained MM in consequence higher.
Response: thank you for the highly valuable scholarly comments and suggestions. Revision was made on the abstract and background section stating that maternal mortality reduction achieved with cervical cancer screening.
1.2. Mention is made “The incidence, death rate and morbidities associated with cervical cancer is significantly varies across the world; higher in the developing nations than compared to the 80 developed countries”. While again it is stated “The prevalence of cervical cancer screening is much higher at the Western countries than SSA” (11, 12); the two statements looks contradictory.
Response: Thank you for the comments, but, the two statements is non-contradictory. Hence, the incidence, death rate and morbidities associated with cervical cancer is significantly varies across the world, which is higher in developing countries like SSA. This is explained due to high prevalence and severity of the problem among in low income countries and the fact that it is the only gynaecologic cancer which can be prevented and treated through early screening and follow-up, and the cervical cancer screening practice in low income countries is significantly low. Therefore, the two statements support each other.
2.1. There is no clarity on whether this review is ‘systematic’ or ‘met-analysis’ or ‘both’. If it is both, it is imperative to clarify which part of it is systematic and meta-analysis OR clarify why both were considered.
Response: Thank you for the valuable comments. We used the PRISMA diagram or recommendations of the systematic review and meta-analysis including the report of this study like the search strategy and the overall written was based on the recommendations. The meta-analysis commands and software were used based on the meta-analysis Cochrane handbooks. The meta-analysis was done to get the pooled estimate using Stata 14 using a meta-analysis written command. To do a good review and meta-analysis it should be searched systematically and other quality measures should be addressed what we have tried.
2.2. From the statement “All published and unpublished studies through April 7, 2020” there were quite few concerns. Firstly what was the lower time frame? Could it be any document from time immemorial to April 7, 2020? Secondly, how were the unpublished reports captured? Was there any criterion set to identify those?
Response: accepted and specific lower time frame was putted (2016) and the criteria used to identify unpublished articles were those fully access during manual search, found in university repositories and those studies fulfilling quality score to be included in this study.
2.3. While WHO’s recommended age of CC screening is 30-50, it is not clear why in this study age 18-49 years was chosen? Is it not contradictory?
Response: Thank you for the highly valuable comments. I completely agree what you supposed to do so and revision was made throughout the manuscript. The reproductive age group is not representative for all the all age eligible women for cervical cancer screening for the population charactertics we included. The recommendation was for the general population Evidence show success of cervical screening initiatives depend on high participation of the target population, which in turn is determined by the women’s knowledge, perceptions, health orientations and other socio-cultural issues. It is also affected by factors including early marriage, early sexual practice, delivery of the first baby before the age of 20, too many or too frequent childbirths, multiple sexual partners and low socio economic status. Women with early sexual practice, multiple partners, having HIV AIDS and sexual transmitted disease should have more screening schedule.
According to world health organization (WHO) guideline, every sexually active woman aged 30–49 years should undergo cervical cancer screening at least every 5 years. However, sexually active and HIV-positive women are suggested to be screened every 3 years regardless of their age. HIV positive women Ethiopia adopted the WHO recommendation in 2015 and recommended HIV positive women to start screening at HIV diagnosis, regardless of age once the woman is sexually exposed. In this meta-analysis age all age eligible women or from different population charactertics for cervical cancer screening such as women from 30-50 years old, HIV positive women, healthcare workers, and commercial sex workers were included. Thus, eligible women are better than reproductive age and we have accepted your comment.
#3. Results
3.1. The studies were drawn from five geographic regions: Addis Ababa, Amhara, Southern Nations, Nationalities and Peoples, Oromia and Tigray with only one from the national- level study. Couple of concern here. Firstly, how was the 18,067 women considered to estimate the pooled… proportionated in light of population size. Given the fact that studies are not proportional to the population of the regions, it would be difficult to reach conclusion as desired – this is about comparability of results. Secondly, I am wondering if this study could mirror realities for the country at large. Perhaps clarifying those and stating limitations may help.
Response: accepted and revision was made. The limitations were stated in regard to the less representativeness of five studies out of nine regions in Ethiopia in our meta-analysis.
3.2. I am not convinced that what are stated as ‘most common reasons that hinder the use of cervical cancer screening’ in the result section and conclusion section are aligned. This needs to be checked against the finding and corrected
Response: thank you for the comments suggest being.
We have checked it and the barriers in the result section and conclusion section are aligned
#4. Discussion
4.1. The fact that it was not clear on what of this review is Meta and systematic, the discussion suffers much missing what is being discussed. Perhaps with clarification on how the two contributed to this review may help refine the discussion section.
Response: Highly valuable comment, I completely agree what you supposed and revision was made. In the last two paragraphs of the discussion section narrates about the meta-analysis and systematic review mainly the strength and weakness.
Reviewer #2
1. Generally a good paper, congratulations, however, the work needs some grammatical revision for clarity. I have listed some below but kindly revise the entire paper checking for grammatical and punctuation errors.
Response: Thank you for your scholarly comments.
The major grammatical errors were revised and seen by sinor experts.
2. Line 74- update the reference and use more recent data than 2013
Response: Accepted and data published in 2016 by WHO and Bruni et al 2017 was cited.
3. Line 77- Be consistent in presenting figures i.e. 311000 should have a comma as with other figures
4. Response: accepted and revision was made. Comma as with other figures is putted.
5. Line 78- Correct the grammar of the sentence which starts as "The incidence, death ......"
Response: accepted and the grammar error was revised.
6. Line 85-6- Correct the grammar of the sentence, Line 97-98- Correct grammar, Line 99-100- Correct grammar, Line 103- Correct the punctuation, Line 292-295- Sentence needs revision for clarity, attend to the grammar, Line 295-298- Sentence needs some revision for clarity.
Response: all grammar and punctuation errors was corrected
7. Line 307 - Clarify what "tall reproductive age" refers, sentence may need some revisions
Response: valuable comment and revised. The editing "tall reproductive age" is an error, we want to instead want to spell as all reproductive age and revision was made. Fortunately, hence, it was not clear for reader we remove from the document.
8. Line 309- Add reference of relevant papers to support your interpretation
Response: reference number 73 was cited.
9. Line 367- Replace "representative" with representativeness
10. Response: representative" was replaced by with representativeness.
Submitted filename: Point by Point reponse .docx
Decision Letter 1
Gizachew tessema.
19 Oct 2021
Cervical cancer screening utilization and predictors among eligible women in Ethiopia: a systematic review and meta-analysis
PONE-D-20-22948R1
Dear Mr Desta,
We’re pleased to inform you that your manuscript has been judged scientifically suitable for publication and will be formally accepted for publication once it meets all outstanding technical requirements.
Within one week, you’ll receive an e-mail detailing the required amendments. When these have been addressed, you’ll receive a formal acceptance letter and your manuscript will be scheduled for publication.
An invoice for payment will follow shortly after the formal acceptance. To ensure an efficient process, please log into Editorial Manager at http://www.editorialmanager.com/pone/ , click the 'Update My Information' link at the top of the page, and double check that your user information is up-to-date. If you have any billing related questions, please contact our Author Billing department directly at [email protected] .
If your institution or institutions have a press office, please notify them about your upcoming paper to help maximize its impact. If they’ll be preparing press materials, please inform our press team as soon as possible -- no later than 48 hours after receiving the formal acceptance. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information, please contact [email protected] .
Gizachew Tessema, PhD
Academic Editor
Additional Editor Comments.
I would suggest to shorten the description related to key words and search terms. Instead put the details search terms and key words presented in lines 158-172 in a supplementary appendix. Revise the statement in the methods section of the abstract. Indicate that databases were searched for peer-review articles whereas Google scholar was used to search grey literature
1. If the authors have adequately addressed your comments raised in a previous round of review and you feel that this manuscript is now acceptable for publication, you may indicate that here to bypass the “Comments to the Author” section, enter your conflict of interest statement in the “Confidential to Editor” section, and submit your "Accept" recommendation.
Reviewer #1: All comments have been addressed
Reviewer #2: (No Response)
2. Is the manuscript technically sound, and do the data support the conclusions?
3. Has the statistical analysis been performed appropriately and rigorously?
4. Have the authors made all data underlying the findings in their manuscript fully available?
Reviewer #1: (No Response)
5. Is the manuscript presented in an intelligible fashion and written in standard English?
6. Review Comments to the Author
Reviewer #1: Authors revised the manuscript following the comments. They considered the comments useful which helped them to refine the manuscript
Reviewer #2: Great paper that contribute to knowledge in LMICs. Please see a few comments below:
-Some grammar and punctuation corrections are needful throughout the paper to aid clarity
-Line 74 Use more recent data e.g GLOBOCAN 2020
-Line 77 Be consistent in presentation of figures use the format 311,000
7. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
Reviewer #1: Yes: Mirgissa Kaba, School of Public Health, Addis Ababa University
Reviewer #2: Yes: Oscar Tapera
Acceptance letter
26 Oct 2021
Dear Dr. Desta:
I'm pleased to inform you that your manuscript has been deemed suitable for publication in PLOS ONE. Congratulations! Your manuscript is now with our production department.
If your institution or institutions have a press office, please let them know about your upcoming paper now to help maximize its impact. If they'll be preparing press materials, please inform our press team within the next 48 hours. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information please contact [email protected] .
If we can help with anything else, please email us at [email protected] .
Thank you for submitting your work to PLOS ONE and supporting open access.
PLOS ONE Editorial Office Staff
on behalf of
Dr. Gizachew Tessema
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data availability statement.
- View on publisher site
- PDF (2.8 MB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
Cervical cancer in Ethiopia: survival of 1,059 patients who received oncologic therapy
Affiliations.
- 1 Department of Gynaecology and Institute of Clinical Epidemiology, Martin Luther University, Halle an der Saale, Germany; School of Public Health, Departments of Pathology and Gynaecology, and Radiotherapy Center, School of Medicine, Addis Ababa University, Addis Ababa, Ethiopia; Department of Epidemiology, School of Public Health, Boston University, Boston, Massachusetts, USA [email protected].
- 2 Department of Gynaecology and Institute of Clinical Epidemiology, Martin Luther University, Halle an der Saale, Germany; School of Public Health, Departments of Pathology and Gynaecology, and Radiotherapy Center, School of Medicine, Addis Ababa University, Addis Ababa, Ethiopia; Department of Epidemiology, School of Public Health, Boston University, Boston, Massachusetts, USA.
- PMID: 24951611
- PMCID: PMC4077439
- DOI: 10.1634/theoncologist.2013-0326
Background: Almost 500,000 women are newly diagnosed with cervical cancer (CC) every year, the majority from developing countries. There is little information on the survival of these patients. Our primary objective was to evaluate consecutive CC patients presenting over 4 years at the only radiotherapy center in Ethiopia.
Methods: All patients with CC from September 2008 to September 2012 who received radiotherapy and/or surgery were included (without brachytherapy). Vital status was obtained through telephone contact or patient cards.
Results: Of 2,300 CC patients, 1,059 patients with standardized treatment were included. At the end of the study, 249 patients had died; surviving patients had a median follow-up of 16.5 months; the 10% and 90% percentiles were 3.0 and 32.7 months, respectively. Mean age was 49 years (21-91 years). The majority of patients presented with International Federation of Gynecology and Obstetrics stage IIb-IIIa (46.7%). Because of progression during the waiting time (median 3.8 months), this proportion declined to 19.3% at the beginning of radiotherapy. The 1- and 2-year overall survival probabilities were 90.4% and 73.6%. If assuming a worst-case scenario (i.e., if all patients not available for follow-up after 6 months had died), the 2-year survival probability would be 45.4%.
Conclusion: This study gives a thorough 4-year overview of treated patients with CC in Ethiopia. Given the limited treatment availability, a relatively high proportion of patients survived 2 years. More prevention and early detection at all levels of the health care system are needed. Increasing the capacity for external-beam radiation as well as options for brachytherapy would facilitate treatment with curative intention.
Keywords: Africa; Ethiopia; Prognosis; Survival; Uterine cervical neoplasms.
©AlphaMed Press.
Publication types
- Research Support, Non-U.S. Gov't
- Cohort Studies
- Disease-Free Survival
- Ethiopia / epidemiology
- Middle Aged
- Neoplasm Staging
- Uterine Cervical Neoplasms / mortality*
- Uterine Cervical Neoplasms / pathology
- Uterine Cervical Neoplasms / therapy*

IMAGES
COMMENTS
Apr 15, 2024 · Nearly 99% of cervical cancer is caused by the human papillomavirus (HPV) and it is largely preventable [5].The World Health Organization (WHO) Director-General announced a global cervical cancer elimination program [6] and launched a global strategy to accelerate elimination in 2020 [6].
Cervical cancer continues to be a major public health problem affecting thousands of women in Ethiopia. As the disease is purely preventable, classic cervical cancer prevention strategies that include HPV vaccination using a broad genotype coverage, screening using a high precision test, and treatin …
Jan 15, 2022 · Background Cervical cancer is one of the most common malignancies affecting women worldwide with large geographic variations in prevalence and mortality rates. It is one of the leading causes of cancer-related deaths in Ethiopia, where vaccination and screening are less implemented. However, there is a scarcity of literature in the field. Therefore, the objective of this review was to describe ...
If it is leg, it may be cut by doctors and the patient may be cured if it is not disseminated to other body parts. However, I don’t know what is done for cervical cancer (26 years old married women). Cancer treatment is with drug or injection which can be given for longer period of time. The same is true for cervical cancer.
Cervical cancer incidence, death, and prevalence were 17.3%, 16.5%, and 18.2% in Ethiopia, respectively. 2 Cervical cancer prevalence rates in Ethiopian women per 100 000 people per year are projected to be 23%. 5 Cervical cancer was confirmed to be the second most common cancer diagnosed in Ethiopian adult women, after breast cancer. 4,6,7
Jan 4, 2022 · Research on cervical cancer interventions in Ethiopia has focused almost exclusively on women’s awareness and knowledge of cervical cancer and screening [8, 16, 18, 22, 23], and to a lesser extent on provider perspectives on screening [17, 23, 24].
Oct 15, 2022 · Introduction HPV vaccination of adolescent girls is the primary strategy for cervical cancer prevention but in Ethio-pia, it lacks emphasis. Despite different studies done and found a highly ...
Nov 12, 2019 · Purpose. Cervical cancer remains the second most common cancer and cancer-related death among women in Ethiopia. This is the first study, to our knowledge, describing the demographic, and clinicopathologic characteristics of cervical cancer cases in a mainly rural, Southwestern Ethiopian population with a low literacy rate to provide data on the cervical cancer burden and help guide future ...
Regional variation in the burden of cervical cancer screening in Ethiopia might be explained by the difference in maternal health care service utilization that could be explained by in the difference in spousal support, cultural and linguistic diversity across the regions and societal stigmatization.
Jun 4, 2021 · Background: Almost 500,000 women are newly diagnosed with cervical cancer (CC) every year, the majority from developing countries. There is little information on the survival of these patients. Our primary objective was to evaluate consecutive CC patients presenting over 4 years at the only radiotherapy center in Ethiopia.