Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Find in topic

RELATED TOPICS
A 47-year-old woman was found to have hyperglycemia at a health fair when a random blood glucose level was 227 mg/dL (12.6 mmol/L). Several days later, a fasting blood glucose value was 147 mg/dL (8.2 mmol/L). She has no previous history of diabetes, is alarmed by the possibility of having this disorder, and seeks your advice.
The patient has been treated for hypertension for 10 years, currently with amlodipine 10 mg by mouth daily. She was once told that her cholesterol value was "borderline high" but does not know the value.
She denies symptoms of diabetes, chest pain, shortness of breath, heart disease, stroke, or circulatory problems of the lower extremities.
She estimates her current weight at 165 lbs (75 kg). She thinks she weighed 120 lbs (54 kg) at age 21 years but gained weight with each of her three pregnancies and did not return to her nonpregnant weight after each delivery. She weighed 155 lbs one year ago but gained weight following retirement from her job as an elementary school teacher. No family medical history is available because she was adopted. She does not eat breakfast, has a modest lunch, and consumes most of her calories at supper and in the evening.
On examination, blood pressure is 140/85 mmHg supine and 140/90 mmHg upright with a regular heart rate of 76 beats/minute. She weighs 169 lbs, with a body mass index (BMI) of 30.9 kg/m 2 . Fundoscopic examination reveals no evidence of retinopathy. Vibratory sensation is absent at the great toes, reduced at the medial malleoli, and normal at the tibial tubercles. Light touch sensation is reduced in the feet but intact more proximally. Knee jerks are 2+ bilaterally, but the ankle jerks are absent. The examination is otherwise within normal limits.
Type 2 diabetes: a case study
Affiliation.
- 1 Queen's University Belfast, Belfast, Northern Ireland.
- PMID: 25270482
- DOI: 10.7748/ns.29.5.37.e9142
Increased prevalence of diabetes in the community has been accompanied by an increase in diabetes in hospitalised patients. About a quarter of these patients experience a hypoglycaemic episode during their admission, which is associated with increased risk of mortality and length of stay. This article examines the aetiology, pathophysiology, diagnosis and treatment of type 2 diabetes using a case study approach. The psychosocial implications for the patient are also discussed. The case study is based on a patient with diabetes who was admitted to hospital following a hypoglycaemic episode and cared for during a practice placement. The importance of early diagnosis of diabetes and the adverse effects of delayed diagnosis are discussed.
Keywords: Blood glucose; case study; diabetes; glucose testing; hyperglycaemia; hypoglycaemia; insulin resistance; sulfonylureas; type 2 diabetes.
Publication types
- Case Reports
- Anxiety / complications
- Depression / complications
- Diabetes Mellitus, Type 2 / diagnosis*
- Diabetes Mellitus, Type 2 / physiopathology
- Diabetes Mellitus, Type 2 / therapy
- Hypoglycemic Agents / therapeutic use
- Middle Aged
- Hypoglycemic Agents
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Case Study: Remission of Type 2 Diabetes After Outpatient Basal Insulin Therapy
Sierra c schmidt, martha ann huey, heather p whitley.
- Author information
- Copyright and License information
Corresponding author: Heather P. Whitley, [email protected]
Corresponding author.
Readers may use this article as long as the work is properly cited, the use is educational and not for profit, and the work is not altered. See http://creativecommons.org/licenses/by-nc-nd/3.0 for details.
Diabetes is a chronic, progressive disease with potentially serious sequelae. Treatment for type 2 diabetes often begins with oral agents and eventually requires insulin therapy. As the disease progresses, drug therapies are often intensified and rarely reduced to control glycemia. Conversely, in type 1 diabetes, some patients experience a “honeymoon period” shortly after diagnosis, wherein insulin needs decrease significantly before intensification is needed ( 1 ). No comparable honeymoon period has been widely described for type 2 diabetes. However, a few studies have demonstrated that drug-free glycemic control can be achieved in type 2 diabetes for 12 months on average after a 2-week continuous insulin infusion ( 2 – 4 ). Here, we describe an unusual case of a 26-month drug holiday induced with outpatient basal insulin in a patient newly diagnosed with type 2 diabetes.

Case Presentation
A 69-year-old white woman (weight 72.7 kg, height 59 inches, BMI 32.3 kg/m 2 ) was diagnosed with type 2 diabetes in June 2011. She presented with an A1C of 17.6% (target <7%) and a fasting blood glucose (FBG) of 452 mg/dL (target 70–130 mg/dL). Before diagnosis, the patient had not used any oral or parenteral steroids nor had she experienced any traumatic physical or emotional event or illness that could have abruptly increased her blood glucose. Metformin 500 mg twice daily was initiated at diagnosis, but was discontinued 9 days later to avoid risk of lactic acidosis, as her serum creatinine was 1.5 mg/dL. At that time, her fasting self-monitoring of blood glucose (SMBG) values ranged from 185 to 337 mg/dL. Treatment with 25 units of insulin detemir daily (0.34 units/kg/day) was initiated in place of metformin. The patient was counseled on diet modifications and encouraged to exercise.
One month later (July 2011), the patient’s fasting SMBG values had improved to a range of 71–212 mg/dL with a single hypoglycemic episode (58 mg/dL); her weight and BMI increased slightly to 74.1 kg and 32.9 kg/m 2 , respectively. Hypoglycemia education was reinforced, and insulin therapy was switched from 25 units of detemir delivered with the Levemir FlexPen to 28 units (0.38 units/kg/day) of insulin glargine delivered with the Lantus SoloStar due to the patient’s preference for this device. Two weeks later, the patient reported continued improvements in fasting SMBG (70–175 mg/dL) with one hypoglycemic episode (67 mg/dL). In response to the hypoglycemic episode, her insulin glargine dose was decreased to 25 units daily.
In September, the patient reported fasting SMBG values ranging between 71 and 149 mg/dL, and her A1C was 7.9%. On days when the patient skipped lunch, her midday blood glucose level would drop to <70 mg/dL (54–60 mg/dL). She was counseled not to skip meals, and her insulin glargine dose was maintained.
In October, the patient’s weight was 71.4 kg, and her BMI was 31.7 kg/m 2 . She reported recently initiating a cinnamon supplement and switching her beverage intake from sugar-sweetened products to water and diet soda. Although the majority of her fasting SMBG values were controlled (80–110 mg/dL), she had experienced six hypoglycemic episodes (FBG 13–64 mg/dL). All values were objectively confirmed in the patient’s glucose meter, and the meter was replaced in case of device error. Her daily insulin glargine dose was decreased to 20 units (0.28 units/kg/day).
In December, her SMBG values ranged between 70 and 106 mg/dL preprandially and 111 and 207 mg/dL postprandially, and she had had six additional hypoglycemic episodes (42–66 mg/dL). The patient’s weight remained stable at 71.4 kg (BMI 31.7 kg/m 2 ). At this follow-up visit, her daily insulin glargine dose was decreased further to 15 units (0.21 units/kg/day).
The patient self-discontinued daily insulin glargine in March 2012 but continued using the cinnamon supplements. She continued to perform SMBG 1–3 times/day, anticipating loss of glycemic control. During the next 2 years, her A1C remained stable (from 6.3% in January 2012 to 6.9% in May 2014) ( Figure 1 ).
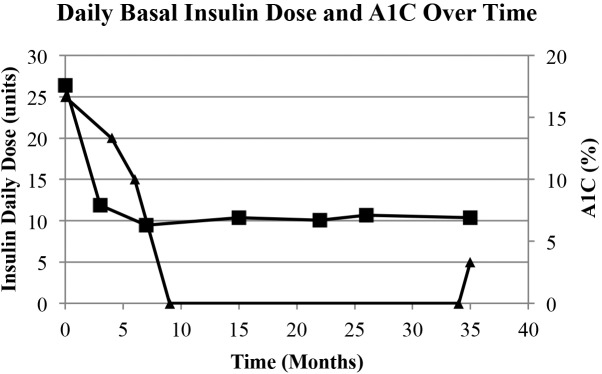
Daily basal insulin dose and A1C over time. Black triangle = insulin units; black square = A1C.
At a follow-up visit in May 2014, the patient’s SMBG indicated a need for resumed drug therapy (FBG 107–169 mg/dL, postprandial blood glucose 108–328 mg/dL). Her weight at this time was 65.5 kg (BMI 29.1 kg/m 2 ). Insulin glargine was reinitiated at 5 units daily (0.08 units/kg/day).
During the drug-free period of March 2012 to May 2014, the patient maintained her lack of sugar-sweetened beverage consumption. However, she reported having difficulties purchasing healthy food options because of financial constraints. In August 2013, she was specifically encouraged to incorporate physical activity (walking) into her daily routine. The patient’s weight during the drug-free interval declined from 70 kg in March 2012 to 65.5 kg in May 2014.
Hyperglycemia causes pancreatic β-cell toxicity, leading to decreased insulin release ( 3 ). In type 1 diabetes, the honeymoon period occurs when residual pancreatic β-cell function is partially restored for an average of 7.2 months, as hyperglycemic stress is removed before the β-cells are ultimately destroyed ( 1 , 3 ).
Past studies demonstrated induction of a drug-free period when patients newly diagnosed with type 2 diabetes were treated with 2–3 weeks of intensive insulin therapy ( 2 – 5 ). Ilkova et al. ( 2 ) induced a 12-month drug-free period in 46.2% ( n = 6) of patients using an insulin infusion averaging 0.61 units/kg/day. Three patients maintained glycemic control for 37–59 months. Li et al. ( 3 ) also induced a 12-month drug-free period in 47.1% ( n = 32) of patients with an insulin infusion of 0.7 units/kg. Additional studies indicate that basal-bolus insulin therapy (0.37–0.74 units/kg/day) using NPH and regular insulin can also induce a 12-month drug-free period in a similar percentage of patients (43.8–44.9%) ( 4 , 5 ).
The mechanism of remission appears to be related to resumption of endogenous insulin production after glucotoxicity is resolved. Glucotoxicity has been shown to inhibit first-phase insulin secretion from the pancreatic β-cells ( 3 ). Li et al. ( 3 ) theorized that an insulin infusion corrects hyperglycemia and removes stress from the β-cells, allowing them to produce insulin, resulting in euglycemia. Their study quantified an increase in secretion of endogenous insulin (44%) and C-peptide (26%) after 2 weeks of continuous insulin infusion. The mechanism through which insulin induces a period of drug-free glycemic control in type 2 diabetes appears to be similar to that causing the honeymoon period in type 1 diabetes.
To our knowledge, this is the first report of basal insulin monotherapy–induced remission of type 2 diabetes. Previous studies required multiple daily injections in a basal-bolus therapy regimen using NPH and regular insulin or hospitalization of patients administered a continuous insulin infusion ( 2 – 5 ).
Basal-only insulin therapy may be a slower method of achieving remission compared to more intensive insulin regimens. In this case, basal insulin was maintained for 9 months. However, according to the FBG trend, discontinuation could have occurred sooner. This report suggests that a trial of basal insulin dosed at 0.2–0.3 units/kg/day, with follow-up every 2–4 weeks in severely hyperglycemic patients with newly diagnosed type 2 diabetes, may be an alternative method to achieving temporary remission. Although this insulin regimen requires a longer timeframe compared to remission induced by basal-bolus therapy or continuous insulin infusion, it provides a more convenient outpatient therapeutic option at a lower cost.
Limitations of this case study include the patient’s use of cinnamon supplementation, which was continued throughout the drug-free period. Although reports are conflicting regarding its efficacy in type 2 diabetes, it is possible that cinnamon may have exerted a mild antidiabetic effect. Positive cinnamon studies have demonstrated a 0.36% A1C reduction after 3 months of use ( 6 ). Additionally, the patient’s weight declined by 3.75% during the 9 months of basal insulin therapy, which was likely in response to introducing dietary modifications related to beverage consumption. Most studies suggest that an A1C reduction of 0.36% ( 7 ) to 0.66% ( 8 ) can be achieved with intensive lifestyle interventions. Therefore, it is unlikely that cinnamon in combination with the mild lifestyle modifications accounted for a nearly 11% A1C reduction from baseline.
Eliminating the consumption of sugar-rich beverages alters the postprandial glycemic curve. In clinical practice, suppressing postprandial blood glucose excursions by adopting significant dietary improvements may postpone or obviate the need for bolus insulin therapy. Likewise, the remission of diabetes potentially may be achieved, as seen in this case, with monotherapy basal insulin when dietary modifications significantly alter the postprandial glycemic curve. However, it is unknown whether remission can be achieved using basal insulin administration alone in patients who choose not to incorporate lifestyle modifications or in patients with baseline healthy eating and exercise habits.
Although weight changes did not appear to contribute to disease remission, the moderate weight loss (6.5%) achieved during the drug-free interval and continued SMBG both may have contributed to maintaining and extending the remission period. The Diabetes Prevention Program ( 9 ) showed that lifestyle modifications aimed at achieving a 7% reduction of weight significantly delay the onset of diabetes compared to placebo and metformin. Finally, performing SMBG through the drug-free period may have empowered the patient by providing objective criteria necessary to validate the benefits of lifestyle modifications.
Based on this case, it is possible that initial type 2 diabetes management with basal insulin can temporarily restore β-cell function to a degree to which blood glucose control can be maintained without drug therapy. Although previous studies conducted with intensive insulin regimens have reported response rates nearing 50% for ∼12 months ( 2 – 5 ), future studies should investigate the ideal basal dose, percentage of patient responders, duration of drug-free glycemic control, and mechanism through which this phenomenon occurs. This case further highlights the need to educate every newly diagnosed patient about the treatment of hypoglycemic events.
The purposeful remission of diabetes is not widely attempted or generally considered possible. Although literature exists regarding the temporary honeymoon period experienced after insulin initiation in some people with type 1 diabetes ( 1 ), comparatively little research is available regarding the influence of insulin on the remission of type 2 diabetes. Current literature suggests benefit in nearly 50% of patients newly diagnosed with type 2 diabetes using one of the following strategies: a 2-week inpatient insulin infusion or multiple daily injections of basal-bolus therapy ( 2 – 5 ). However, there are disadvantages to these methods. A continuous insulin infusion requires inpatient admission, whereas a basal-bolus insulin regimen requires purchase of two products and administration of multiple subcutaneous injections daily. Unfortunately, both methods may be impractical, costly, and inconvenient for many patients newly diagnosed with type 2 diabetes.
This case outlines a third potential option for inducing remission of type 2 diabetes: basal insulin monotherapy. Using this approach avoids the costly and inconvenient hospital admission required for the continuous insulin infusion strategy. Furthermore, the cost of drug therapy is reduced with the purchase of one rather than two insulin products, as needed in a basal-bolus insulin regimen. Additionally, using basal insulin alone reduces the risk of hypoglycemic events that may occur with stacking of multiple insulin products. Finally, requiring only one injection of insulin each day offers a more manageable alternative for newly diagnosed patients compared to the multiple daily injections required with a basal-bolus insulin regimen.
By using this basal insulin strategy, the patient in this case was able to achieve drug-free glycemic control for 26 months. Early initiation of basal insulin monotherapy in patients newly diagnosed with type 2 diabetes is a more convenient and cost-effective approach than methods previously described and could potentially induce remission of type 2 diabetes in other patients.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
- 1. Abdul-Rasoul M, Habib H, Al-Khouly M. The ‘honeymoon phase’ in children with type 1 diabetes mellitus: frequency, duration, and influential factors. Pediatr Diabetes 2006;7:101–107 [ DOI ] [ PubMed ] [ Google Scholar ]
- 2. Ilkova H, Glaser B, Tunckale A, Bagriacik N, Cerasi E. Induction of long-term glycemic control in newly diagnosed type 2 diabetic patients by transient intensive insulin treatment. Diabetes Care 1997;20:1353–1356 [ DOI ] [ PubMed ] [ Google Scholar ]
- 3. Li Y, Xu W, Liao Z, et al. . Induction of long-term glycemic control in newly diagnosed type 2 diabetic patients is associated with improvement of β-cell function. Diabetes Care 2004;27:2597–2602 [ DOI ] [ PubMed ] [ Google Scholar ]
- 4. Weng J, Li Y, Xu W, et al. . Effect of intensive insulin therapy on β-cell function and glycaemic control in patients with newly diagnosed type 2 diabetes: a multicentre randomised parallel-group trial. Lancet 2008;371:1753–1760 [ DOI ] [ PubMed ] [ Google Scholar ]
- 5. Ryan EA, Imes S, Wallace C. Short-term intensive insulin therapy in newly diagnosed type 2 diabetes. Diabetes Care 2004;27:1028–1032 [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Akilen R, Tsiami A, Devendra D, Robinson N. Glycated haemoglobin and blood pressure-lowering effect of cinnamon in multi-ethnic type 2 diabetic patients in the UK: a randomized, placebo-controlled, double-blind clinical trial. Diabet Med 2010;27:1159–1167 [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. Wing RR, Bahnson JL, Bray GA, et al. . Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes: four year results of the Look AHEAD Trial. Arch Intern Med 2010;170:1566–1575 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 8. American Diabetes Association Standards of medical care in diabetes—2014. Diabetes Care 2014;37(Suppl. 1):S14–S80 [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. DPP Research Group Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (407.5 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

IMAGES
VIDEO
COMMENTS
The following case study illustrates the clinical role of advanced practice nurses in the management of a patient with type 2 diabetes. Case Presentation A.B. is a retired 69-year-old man with a 5-year history of type 2 diabetes.
In type 2 diabetes, characterized by insulin resistance and insulin deficiency, the pathophysiology of hypertriglyceridemia is an increased hepatic production of triglycerides as well as a decreased lipoprotein lipase activity leading to slower breakdown of VLDL cholesterol and chylomicrons.3 The American Diabetes Association (ADA) Clinical ...
CASE. A 47-year-old woman was found to have hyperglycemia at a health fair when a random blood glucose level was 227 mg/dL (12.6 mmol/L). Several days later, a fasting blood glucose value was 147 mg/dL (8.2 mmol/L). She has no previous history of diabetes, is alarmed by the possibility of having this disorder, and seeks your advice.
M.P. is a 30-year-old man who was diagnosed with type 2 diabetes 2 weeks before admission to the hospital. He has a strong family history of type 2 diabetes. He smokes heavily (> 20 cigarettes/day) and admits to some alcohol consumption. His primary care physician had started him on metformin,500 mg three times daily.
The patient received a diagnosis of type 2 diabetes mellitus; lifestyle modification was recommended. Three months post partum, the glycated hemoglobin level was 5.9% and the BMI was 30.0 ...
Diabetes mellitus currently affects 6.4% or 285 million adults worldwide, and that number is expected to increase to 7.7% or 439 million by 2030. 1 In the United States, the prevalence of diabetes in adults increased from 11.3% in 2010 to 12.3% in 2012. 2 The current type 2 diabetes mellitus (T2DM) epidemic is closely associated with a parallel obesity epidemic, with more than 85% of patients ...
Although type 2 diabetes is considered a chronic disease that is difficult to completely cure7,8, studies have reported complete remission of type 2 diabetes in adults after intensive lifestyle modification.9 Here we report two cases of type 2 diabetes with partial or complete response to lifestyle modification, particularly FM decrease.
This article examines the aetiology, pathophysiology, diagnosis and treatment of type 2 diabetes using a case study approach. The psychosocial implications for the patient are also discussed. The case study is based on a patient with diabetes who was admitted to hospital following a hypoglycaemic episode and cared for during a practice ...
Results. Results of the lunch study for a type 2 diabetic subject indicate that the recovery time of the post-prandial blood glucose level can be adjusted to 4 hours, which is comparable to the typical time interval for non-diabetics: 3 to 4 hours. A moderate lifestyle adjustment of light supper coupled with morning swimming of 20 laps in a 25 ...
However, a few studies have demonstrated that drug-free glycemic control can be achieved in type 2 diabetes for 12 months on average after a 2-week continuous insulin infusion (2 – 4). Here, we describe an unusual case of a 26-month drug holiday induced with outpatient basal insulin in a patient newly diagnosed with type 2 diabetes.